Spirometric profile of people living with HIV on antiretroviral drugs in Abidjan
Abstract
Introduction
People living with HIV (PLHIV) are susceptible to developing non- communicable chronic respiratory diseases. Our objective was to study the spirometric profile of this population.
Material and methods
This was a descriptive and analytical cross-sectional retro-prospective study conducted from March 15 to June 15, 2022 and relating to the analysis of the medical files of asymptomatic and eligible for spirometry PLHIV, aged 18 years and above. They were received in the voluntary counselling and testing (VCT) centres of one of the two pulmonology departments in Abidjan.
Results
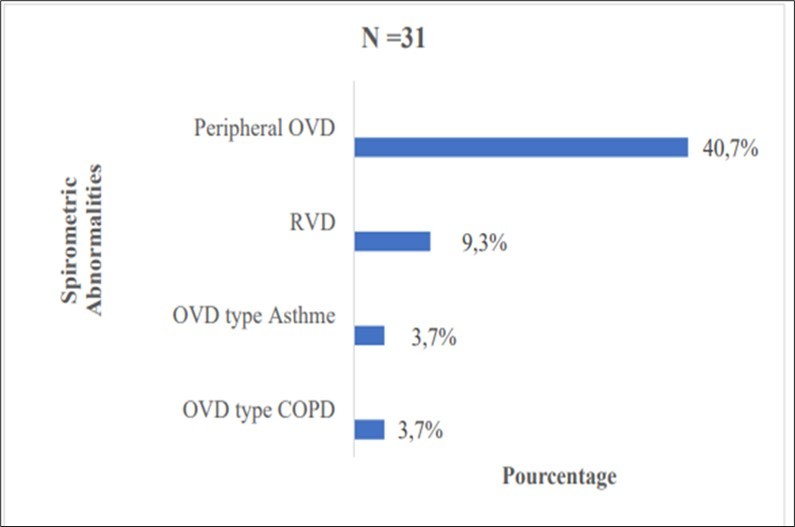
The study involved 54 subjects including 22 men (40.7%) and 32 women (59.3%) with an average age of 48.9 years. The majority of patients were non-smokers (81.4%) and the main history was pulmonary tuberculosis (35.2%). Only 29.6% had chronic respiratory symptoms and 42.6% had a normal BMI. The frequency of spirometric abnormalities was 57.4%. These spirometric abnormalities included 40.7% peripheral obstructive pattern; 9.3% restrictive pattern; 3.7% asthma and 3.7% COPD. A more than 10 years duration of HIV infection (p=0.001 OR= 0.2 (0.1 – 0.7)) and a duration of ART of at least 10 years (p=0.001 OR= 0, 2 (0.1 – 0.7)) were significantly associated with the existence of ventilatory abnormalities.
Conclusion
The high frequency of ventilatory anomalies in PLHIV independently of the existence of chronic respiratory signs leads us to propose spirometry in the follow-up assessment of PLHIV while paying particular attention to those on ARVs for more than 10 years.
Author Contributions
Academic Editor: Sasho Stoleski, Institute of Occupational Health of R. Macedonia, WHO CC and Ga2len CC.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2024 Samake Kadiatou, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
The Human Immunodeficiency Virus (HIV) remains a major public health problem worldwide 1. People living with HIV (PLHIV) are the prerogative of opportunistic infections, the frequency of which is decreasing with the advent of triple antiretroviral therapy and cotrimoxazole prophylaxis. Currently, there is an increase in chronic non-communicable diseases in this population. The prevalence of non-communicable chronic respiratory diseases increased from 11.9 in 2007 to 14.1% in 20132. Among the non-communicable chronic respiratory diseases described in PLHIV, asthma and chronic obstructive pulmonary disease (COPD) are cited as significant factors of morbidity and mortality 3, 4, 5. Several Western studies have pointed out that HIV infection and antiretroviral treatment (ART) can contribute to the development of these diseases in PLHIV 6, 7, 8. Also, HIV is a risk factor for developing chronic obstructive pulmonary disease (COPD), pulmonary arterial hypertension (PAH) and chronic respiratory failure (CRF) 2. Studies conducted in developed countries have shown that the prevalence of obstructive ventilatory defect (OVD) in PLHIV ranged from 7 to 21% 9. This high prevalence of OVD was observed in both children and adults infected with HIV. 5, 7, 10. A history of pulmonary tuberculosis, low CD4 count, prolonged duration of HIV infection and smoking have been identified as factors associated with these ventilatory defects, although the mechanisms are not clearly established 11. In sub-Saharan Africa, the region of the world with the highest proportion of PLHIV, very few studies have focused on spirometric abnormalities within this population. The frequency of spirometric abnormalities was 13% in South Africa and a prevalence of 5.2% of COPD and 5.2% of asthma in Cameroon 12, 13. Due to the additional morbidity that a non-communicable chronic respiratory disease would cause in this population, and given the lack of data on the subject in sub-Saharan Africa, specifically in Côte d'Ivoire, this works’ objective has been set to study the spirometric profile of PLHIV followed in pneumology.
Materials and methods
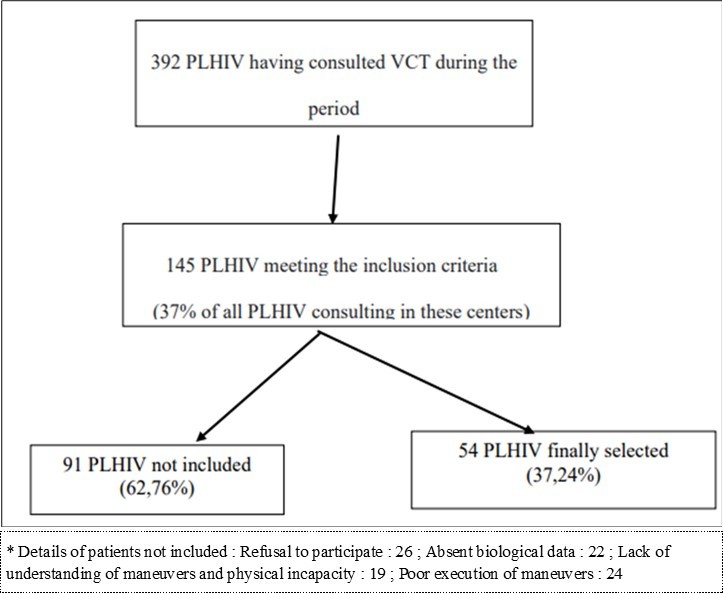
This was a descriptive and analytical retro-prospective cross-sectional study, conducted in the voluntary counselling and testing (VCT) centres, specialized in monitoring PLHIV and supplying them with ART in the pulmonology units of the Cocody and Treichville University Hospital Centres in the district of Abidjan, from March 15 to June 15, 2022. This study concerned PLHIV aged at least 18 years, received in the VCT centres of one of the centres mentioned for the medical follow-up of HIV infection, presenting no acute respiratory or general symptoms (dyspnoea, cough, fever ≤ 3 weeks), no contraindication to performing spirometry according to the ATS/ERS 2019 criteria 14, and having agreed to participate in the study after obtaining informed consent. Were excluded from the study, those with known asthma or COPD (Figure 1). Spirometry was performed in every person included in the study. We used as equipment a 7-inch touch screen portable turbine spirometer with an integrated printer (Spirolab New®) with the accessories (turbine, disposable mouthpiece, an antibacterial filter, nose clip and an inhalation chamber), salbutamol spray dosed at 100 µg and a pulse oximeter. When performing the test, acceptability and repeatability criteria of the parameters were applied according to the ATS/ERS recommendations 14. The reference values were those of the African-American population, taken from the Global Lung Initiative (GLI) 15. The instructions were well explained before any manoeuvre and at least three tests were carried out by the subject with a maximum of eight tests. For hygiene purpose, the material used, in particular the mouthpiece, turbine and antibacterial filter, was single-use and disposable. The spirometric data were interpreted using operational definitions. The diagnosis of COPD was made on the basis of a Tiffeneau index (FEV1/FVC) post bronchodilator less than 0.7 or below the lower limit of normal (LLN) 9, 16. The severity of COPD was assessed by the value of the FEV1; that of asthma was retained on the basis of at least 12% and 200 ml increase in the FEV1 after the inhalation of 400 micrograms of salbutamol through an inhalation chamber 17; the obstruction of the small calibre bronchi was retained before a forced expiratory flow (FEF25-75%) below 65% of the predicted value. A proportional decrease in airflow and lung volume below the LLN with a stable or high Tiffeneau index was suggestive of a restrictive ventilatory defect (RVD) 16. On the other hand, a disproportionate decrease in ventilatory flow and lung volumes below the LLN with a decreased Tiffeneau index was suggestive of a mixed ventilatory defect (OVD with restrictive pattern) 16. Spirometry was considered normal when FVC and FEV1 values were greater than or equal to 80% of the predicted value, a Tiffeneau greater than 0.7 and peripheral flows above 65% of the predicted value 14. Data was collected from the medical records of PLHIV using a standardized and anonymous survey form. These were socio-demographic data (age, sex, profession, level of education), clinical data including history (HIV status, lung infection, smoking), respiratory symptoms and physical examination (height, weight, BMI), biological (CD4 count, viral load) and spirometric parameters (lung flow rates and volumes). Data collected on individualized questionnaires were recorded in CSPRO 7.3 software and then exported to SPSS version 26 for statistical analysis. We performed bivariate analysis using the Chi² test or Fisher's exact test for predicted counts less than 5 to determine factors potentially related to spirometric abnormalities, and logistic regression analysis to identify factors independently associated with spirometric abnormalities. Statistical significance threshold was set at 5% for all analyses.
Results
Socio-demographic characteristics
The study population was composed of 409 women (59.3%) and 356 men (40.7%), with an average age of 48.9 ± 10.8 years with ages ranging from 24 to 79 years. The age group 40 to 50 years represented 42.6%. (Table 1).
PLHIV mostly worked in the informal sector (46.3%), the majority had attended the secondary level of education (37%) followed by the primary level (29.6%).
Table 1. Socio-demographic characteristics of PLHIV| Socio demographic characteristics | Effective (n=54) | % | |
| Age | (20-30) | 3 | 5.6 |
| (30- 40) | 5 | 9.3 | |
| (40 -50) | 23 | 42.6 | |
| (50 -60) | 16 | 29.6 | |
| (60 -70) | 5 | 9.3 | |
| ≥70 years | 2 | 3.76 | |
| Sex | Male | 22 | 40.7 |
| Female | 32 | 59.36 | |
| Age of HIV diagnosis | <5 years | 11 | 20.4 |
| (5 – 10) | 9 | 16.7 | |
| ≥ 10 years | 32 | 59.3 | |
| Duration of ARV treatment | <5 years | 12 | 22.2 |
| (5 – 10) | 10 | 18.5 | |
| ≥ 10 years | 32 | 0.9 | |
| ARV treatment | TDF/3TC/DTG | 42 | 77.8 |
| TDF/3TC/EFV | 7 | 13 | |
| Others* | 5 | 9.4 | |
| Adherence to ARV treatment | Yes | 51 | 94.4 |
| No | 3 | 5.6 | |
Characteristics of HIV infection
The majority (63%) of patients had been known to be PLHIV for at least 10 years with an average seniority of 11.3 ± 5.6 years and a standard deviation of 5.6 years (extremes: 1 – 21 years). All patients were on ART at the time of the study (100%). Among them 59.3% had been on ART for at least 10 years. The average duration of ART was 10.4 ± 5.3 years (extremes: 1 – 21 years). The majority of patients (77.8%) were on the Tenofovir/Lamivudine/Dolutegravir (TLD) triple therapy with good adherence to the ART in 94.4% of cases. (Table 1)
The CD4 count at diagnosis of HIV infection had a median of 240.5 (82.3 – 419) cells/mm3 (range: 1 – 709 cells/mm3). Majority of the patients had moderate immunosuppression (48.1%). The median viral load was 20 (1-50) copies/ml (range: 0 – 306.000 copies/ml) and was detectable in 51.9% of patients. Patients who received cotrimoxazole chemoprophylaxis represented 25.9% compared to 3.7% who received isoniazid.
Clinical features
A history of lung infection was the most common (48.1%). Of these, pulmonary tuberculosis was the most frequent (35.2%). The larger number of our patients were non-smokers (81.4%). Biomass smoke (25.9%) and pesticides (7.4%) were the airborne contaminants to which PLHIV were most exposed. The average duration of exposure to biomass smoke was 24.3 ± 11.1 years and that of exposure to pesticides was 13.9 ± 5.9 years. Chronic respiratory symptoms found in 16 patients (29.6%) were mainly dyspnoea (16.7%) and dry cough (13%). The Body Mass Index (BMI) was normal in 42.6% of patients with an average BMI of 25.5 kg/m2 ± 4.5 kg/m2 (extremes: 17.1 – 35 kg/m2).
Spirometric characteristics
The majority of patients (72.2%) had a normal FEV1 with an average FEV1 of 90.1 ± 16.0% of theoretical (extremes: 64 – 128%). The average FVC was 97.7 ± 15.8% of the theoretical (extremes: 63 – 133%) and 87% of the patients had a normal FVC. The mean Tiffeneau ratio was 77.8 ± 6.5% (range: 56.7 – 91.2%). This ratio was normal in 94.4% of patients. The average FEF25 – 75 was 63.1 ± 22.6% (extremes: 26 – 135%). More than half of the patients (59.3%) had a FEF25 – 75 higher than the norm. The frequency of spirometric abnormalities was 57.4%. Peripheral obstructive ventilatory defect (40.7%) was the most frequent ventilatory anomaly (Figure 2).
Factors associated with spirometric abnormalities
The factors associated with spirometric abnormalities were a more than 10 years duration since the diagnosis of HIV infection (p=0.001 OR= 0.2 (0.1 – 0.7) and an ART of at least 10 years (p=0.001 OR= 0.2 (0.1 – 0.7). However, there was no significant link between socio- demographic characteristics (gender, age, level of education), history of lung infection and smoking, respiratory symptoms, BMI and the presence of spirometric abnormalities (Table 2).
Table 2. Factors associated with spirometric disorders in PLHIV| Variable | Spirometric abnormalities | OR (95% CI) | P- value | ||
| Yes, n (%) | No n (%) | ||||
| Age (years) | |||||
|---|---|---|---|---|---|
| <50 years | 14 (45.2) | 16 (69.5) | 1.1 (0.4- 3.4) | 0.13 | |
| ≥50 years | 17 (54.9) | 6 (26.1) | |||
| Sex | |||||
| Male | 12 (38.7) | 10 (43.5) 13 | 0.8 (0.3- 2.5) | 0.78 | |
| Female | 19 (61.3) | -56.5 | |||
| Level of education | |||||
| < Secondary | 15 (48.4) | 12 (52.2) | 1.1 (0.4- 3.4) | 0.78 | |
| ≥ Secondary | 16 (51.6) | 11 (47.8) | |||
| Length of HIV infection | |||||
| < 10 years | 7 (22.6) | 13 (56.5) | 0.2 (0.1- 0.7) | 0.01 | |
| ≥ 10 years | 24 (77.4) | 10 (43.5) | |||
| ART duration | |||||
| < 10 years | 8 (25.8) | 14 (60.9) | 0.2 (0.1 - 0.7) | 0.01 | |
| ≥ 10 years | 23 (74.2) | 9 (39.1) | |||
| ART combination | |||||
| TDF/3TC/DTG | 25 (80.6) | 17 (73.9) | 1.5 (0.4 - 5.3) | 0.56 | |
| TDF/3TC/EFV | 3 (9.7) | 4 (17.4) | 0.5 (0.1 - 2.5) | 0.44 | |
| Other | 3 (9.7) | 2 (8.7) | 1.1 (0.2 - 7.3) | 1.00 | |
| Viral load | |||||
| Undetectable | 15 (48.4) | 11 (47.8) | 1.1 (0.3 - 3.1) | 0.97 | |
| Detectable | 16 (51.6) | 12 (52.2) | |||
| Initial CD4 count | |||||
| ≤200 | 13 (41.9) | 11 (47.8) | 0.8 (0.3 - 2.3) | 0.67 | |
| >200 | 18 (58.1) | 12 (52.2) | |||
| Smoking | |||||
| Yes | 6(19.4) | 4(17.4) | 1.1 (0.3- 4.6) | 1.00 | |
| No | 25(80.6) | 19(82.6) | |||
| Historyoftuberculosis | |||||
| Yes | 13(76.5) | 6(66.7) | 1.6 (0.3- 9.6) | 0.66 | |
| No | 4(23.5) | 8(33.3) | |||
| Historyofpneumonia | |||||
| Yes | 2(11.8) | 3(33.3) | 0.3(0.1 - 2.1) | 0.30 | |
| No | 15(88.2) | 6(66.7) | |||
| BMI | |||||
| < 25 kg/m² | 16(51.6) | 10(43.5) | 1.4(0.5 - 4.1) | 0.55 | |
| ≥ 25 kg /m² | 15(48.4) | 13(56.5) | |||
| Respiratorysymptoms | |||||
| Yes | 11(35.5) | 5(21.7) | 1.9(0.6 - 6.8) | 0.27 | |
| No | 20(64.5) | 18(78.3) | |||
Discussion
Limits of the study
One of the weaknesses of our study lies in the non-inclusion of 29.65% of cases due to the inability to perform spirometric manoeuvres, responsible for our small sample size. The retrospective component of our study limited the data collected to the sole information available in the patients’ files such as biological data (viral load, CD4 count), some of which were absent. However, the CD4 count and viral load are no longer mandatory for ART initiation. Finally, our analysis of ventilatory function was limited to spirometry. The presence of a RVD in spirometry requires plethysmography for confirmation of this disorder. Despite these limitations, to the best of our knowledge, this study is one of the first in Côte d'Ivoire to assess the ventilatory function of PLHIV. It analysis the profile of spirometric abnormalities observed in PLHIV treated with ARVs.
Socio-demographic characteristics
The mean age of the patients was 48.9 years with a standard deviation of 10.8 years. The age group of 40 to 50 years was the most represented (42.6%). Our results are close to the average age reported in many studies, particularly in the USA 18, South Africa 19 and Cameroon 13 which found an average age of 50, 43.5 and 42.6 years old respectively.
Our study population was mainly composed of women (59.3%) with a sex ratio M/F of 0.68. In the world population and particularly in Côte d'Ivoire, the prevalence of HIV is higher in women than in men 1, 12.
Prevalence of spirometric abnormalities in PLHIV
The frequency of ventilatory anomalies in our study was 57.4%. This is higher than what is found in the literature mainly because of the peripheral OVDs which were not sought in these various studies 13, 19, 5, 18, 20. The prevalence of peripheral OVD was 40.7% in our work. We did not find in the literature a study focusing on this peripheral damage, which would reflect damage to the small bronchi without abnormality of the large bronchi. Particularly in the early forms of COPD, inflammation and structural changes begin and predominate in the distal airways 21. Unlike peripheral OVD, that of asthma was 3.7% in our study population. This frequency is lower than the hospital frequency of 5.2% for asthma found by Pefura-Yone et al. in Cameroon in 2015 13 and at 7% by Van Riel et al in South Africa 19. The frequency of asthma in our study is higher than the 2.99% found by Koffi N et al in Abidjan, Côte d'Ivoire in 200122 and the 2.7% found by Hirani et al in their study 20. The prevalence of COPD in our study population was 3.7%. This proportion was higher than the Ivorian hospital prevalence of COPD found by Anon et al in 2020, which was 2.5% 23. On the other hand, our frequency of COPD was significantly lower than those reported by several African and Western studies where it varied from 5.2 to 27%. 5, 13, 18, 19, 20 This difference could be explained by the higher percentage of smoking patients/former smokers in these different studies than that of our series where the majority of our patients (81.4%) were non- smokers. This high proportion of non-smoking patients is consistent with most studies conducted in sub-Saharan Africa 13, 6, 19, but remains lower than that of Western studies 2, 5, 18, 20, 11. It is already established that smoking is a risk factor or even aetiology of COPD and several studies have demonstrated in their cohort of PLHIV, smoking as a risk factor for the development of non-reversible OVD 13, 5, 18. However, in sub-Saharan Africa, another risk factor to consider in the occurrence of COPD is environmental exposure, particularly to biomass (25.9% in our study). The frequency of RVD in our series (9.3%) is close to that reported by Drummond et al (10%), although slightly higher than that of the general American population of 7% 18. The prevalence of RVD was 38% in Cameroon among PLHIV naïve to ART 24. Given the history of pleuropulmonary infection (48.1%), one would have expected a higher frequency of RVD among the PLHIV in our series. This low frequency of RVD could be related to the almost complete recovery of the lung parenchyma and pleura following these infections, with very few sequelae.
Factors associated with spirometric abnormalities
Previous studies have clearly demonstrated age as a factor associated with spirometric abnormalities in PLHIV 19, particularly in the 40 to 50 years age group 18. This age group was independently associated with the presence of RVD 12. In our series, this link was not significant. Similarly, male sex has been identified as a risk factor for developing spirometric disorders in PLHIV 19, 25, but this association was not significant in our study. Other elements, particularly the low level of education (below secondary) have been described as a factor associated with RVD 26. However, this was not the case in our study. The duration since HIV diagnosis was on average 11.3 years. A less than 13 years average duration of HIV diagnosis was obtained by Gingo et al in the United States 5, but was significantly higher than the 6.25 years obtained by van Riel et al in South Africa 19. Patients with a more than 10 years diagnosis of HIV had significantly more ventilatory abnormalities (p=0.001). Similar observations have been made both in Europe and in Africa. Indeed, Kristoffersen et al in Denmark found an average duration of infection of 9.25 years and a duration of infection greater than 10 years significantly associated with the presence of OVD 27. Drummond et al 11 also found the prolonged duration of HIV infection as a risk factor for developing a ventilatory defect. This increased risk of ventilatory abnormalities with duration of HIV exposure could be explained by direct virus-related pulmonary toxicity, persistent systemic inflammation, altered antioxidant/oxidant balance resulting in oxidative stress, and accelerated immune deterioration. However, ART and duration would also play a role in the occurrence of ventilatory abnormalities. The average duration of ART instituted according to the WHO regimen was 10.4 years. Patients on ART for at least 10 years in our series had significantly more ventilatory abnormalities (p=0.001). TDF+3TC+DTG triple therapy was the most widely used treatment (77.8%) and the majority of our patients (94.4%) were adherent to treatment. Several studies also found an association between the duration of ART and the existence of a ventilatory abnormality. Indeed, Gingo et al in the United States found ART as a risk factor for developing non-reversible OVD. However, the triple therapy used was not specified in this study 5. George et al reported that ART use was independently associated with the development of OVD 10. The link between ART and ventilatory disorders is not known, but potential explanations include the direct effects of ART in the lungs, the restoration of the immune system resulting in a renewed response to subclinical infections and/or the development of auto–immunity. ART-associated cardiovascular diseases, metabolic syndrome, and osteoporosis may be directly linked to antiretroviral agents, particularly protease inhibitors 28, but there are no published reports of antiretroviral drugs and ventilatory disorders. On the other hand, literature notes a link between the degree of immunosuppression and the occurrence of ventilatory anomalies in this population. Several series 5, 7, 10, 11, 29 have found an association between low CD4 count, the high viral load and the development of ventilatory disorders. However, these data may not be applicable to patients with less severe immunodeficiency, as is the case in our study where 48.1% had moderate immunosuppression and an undetectable viral load. Whatever the case, ventilatory anomalies will lead to respiratory manifestations which may vary according to the patient's smoking profile. In our series, the high proportion of non-smokers (81.4%) observed is consistent with most studies conducted in sub-Saharan Africa 13, 6, 19, 26 but remains lower than those of Western studies 2, 5, 18, 20, 11, 29. Indeed, the prevalence of smoking in sub- Saharan Africa in the general population remains lower than that observed in the Western world. It has already been established that smoking is a risk factor or even an aetiology of COPD, but also described as a factor in the development of non-reversible OVD in PLHIV 5, 13, 18. However, in sub-Saharan Africa, another risk factor to consider in the occurrence of COPD is environmental exposure, particularly to biomass (25.9% in our study). A history of pleuropulmonary infection was found in 48.1% of our patients and consisted mainly of pulmonary tuberculosis (35.2%). It has been demonstrated that PLHIV with a history of pulmonary tuberculosis are more at risk of developing RVD 5, 12, 26 and sometimes OVD 13, 19, 29, but the association was not statistically significant, possibly because of our small sample. Indeed, tuberculosis through its sequelae can lead to ventilatory restriction in these patients who are sometimes undernourished or even emaciated. Underweight (defined by a BMI<18.5 kg/m2) was found by certain series to be a risk factor for developing a ventilatory anomaly 6. In our study, we did not find an association between BMI and the presence of ventilatory abnormality. This could be explained by the fact that the majority of our patients had a normal BMI (42.6%). Similarly, only 29.6% complained of chronic respiratory symptoms despite the high prevalence of ventilatory abnormalities. Gingo et al as well as Drummond et al had also found a discrepancy between patient complaints and the presence of ventilatory abnormalities 18, 30. This would mean that one should not always wait for the complaint of dyspnoea or chronic cough to consider spirometry for a PLHIV. Spirometry should therefore be part of the respiratory assessment of PLHIV whether they have chronic respiratory symptoms or not. However, the profile of these patients should be well defined.
Conclusion
The high frequency of ventilatory abnormalities in PLHIV independently of the existence of chronic respiratory symptoms leads us to propose spirometry in the assessment of PLHIV. Particular attention should be paid to PLHIV treated for more than 10 years with ARTs in view of the risk of developing these ventilatory disorders. A larger-scale study would better define the profile of PLHIV who should benefit from this routine spirometry.
References
- 2.Maitre T, Cottenet J, Beltramo G, Piroth L, Bonniaud P et al. (2007) Emergence des pathologies pulmonaires non infectieuses chez les patients vivant avec le virus de l’immunodéficience humaine (VIH) : étude sur la base nationale des données du PMSI de.
- 3.Crothers K, Thompson B W, Burkhardt K, Morris A, Flores S C et al. (2011) HIV- associated lung infections and complications in the era of combination antiretroviral therapy. Proc Am Thorac Soc. 8(3), 275-81.
- 4.Gingo M R, Wenzel S E, Steele C, Kessinger C J, Lucht L et al. (2012) Asthma diagnosis and airway bronchodilator response in HIV-infected patients. , J Allergy Clin Immunol 129(3), 708-714.
- 5.Gingo M R, George M P, Kessinger C J, Lucht L, Rissler B et al. (2010) Pulmonary function abnormalities in HIV-infected patients during the current antiretroviral therapy era. Am J Respir Crit Care Med. 182(6), 790-6.
- 6.MRJ Varkila, Vos A G, Barth R E, Tempelman H A, WLJ Devillé et al. (2019) The association between HIV infection and pulmonary function in a rural African population. PloS One. 14(1), 0210573.
- 7.Drummond M B, Kirk G D, Astemborski J, Marshall M M, Mehta S H et al. (2012) Association between obstructive lung disease and markers of HIV infection in a high- risk cohort. Thorax. 67(4), 309-14.
- 8.Diaz P T, Wewers M D, Pacht E, Drake J, Nagaraja H N et al. (2003) Respiratory Symptoms Among HIV-Seropositive Individualsa. Chest. 123(6), 1977-82.
- 9. (2021) Global Initiative for Chronic Obstructive Lung Disease [Internet]. Global Initiative for Chronic Obstructive Lung Disease - GOLD. [cited. Available from: https://goldcopd.org/
- 10.George M P, Kannass M, Huang L, Sciurba F C, Morris A. (2009) Respiratory symptoms and airway obstruction in HIV-infected subjects in the HAART era. PloS One. 4-7.
- 11.Drummond M B, Merlo C A, Astemborski J, Kalmin M M, Kisalu A et al. (2013) The effect of HIV infection on longitudinal lung function decline among IDUs: a prospective cohort. AIDS Lond Engl. 27-8.
- 12.Drummond M B, Zhao E, Wong M, Kirk G D, Rom W N et al. (2014) Prevalence Of Spirometric Abnormalities Among Hiv-Infected Individuals. Am J Respir Crit Care Med. 189-1196.
- 13.Pefura-Yone E W, Fodjeu G, Kengne A P, Roche N, Kuaban C. (2015) Prevalence and determinants of chronic obstructive pulmonary disease in HIV infected patients in an African country with low level of tobacco smoking. Respir Med. 109(2), 247-54.
- 14.Graham B L, Steenbruggen I, Miller M R, Barjaktarevic I Z, Cooper B G et al. (2019) Standardization of Spirometry. 70-88.
- 15.Quanjer P H, Stanojevic S, Cole T J, Baur X, Hall G L et al. (2012) Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J. European Respiratory Society. 40(6), 1324-43.
- 16.Pellegrino R, Viegi G, Brusasco V, Crapo R O, Burgos F et al. (2005) Interpretative strategies for lung function tests. Eur Respir J. European Respiratory Society. 26(5), 948-68.
- 17. (2021) GINA Main Report [Internet]. Global Initiative for Asthma - GINA. [cited. Available from: https://ginasthma.org/gina-reports/
- 18.Drummond M B, Huang L, Diaz P T, Kirk G D, Kleerup E C et al. (2015) Factors associated with abnormal spirometry among HIV-infected individuals. AIDS. 29(13), 1691-700.
- 19.Riel SE van, Klipstein-Grobusch K, Barth R E, Grobbee D E, Feldman C et al. (2021) Predictors of impaired pulmonary function in people living with HIV in an urban African setting. , South Afr J HIV Med 22-1.
- 20.Hirani A, Cavallazzi R, Vasu T, Pachinburavan M, Kraft W K et al. (2011) Prevalence of obstructive lung disease in HIV population: A cross sectional study. Respir Med. 105(11), 1655-61.
- 21.Chaouat A, Chabot F, Dusser D. (2011) Symptômes et histoire naturelle de la BPCO : rôle des voies aérienne distales. Rev Mal Respir. 28-8.
- 22.Koffi N, Kouassi A B, Horo K, Gondola P, Aka-danguy E. (2001) Profil de l’asthmatique adulte suivi en consultation en milieu africain à Abidjan. Médecine d'Afrique noire. 48-11.
- 23.Anon J C, Dembele R, Toh-Bi Y, Yeo L, Dje-Bi H et al. (2020) Contribution pour améliorer la prise en charge de la BPCO en Afrique noire. , Rev Mal Respir Actual 12(1), 196-7.
- 24.EWP one, Balkissou A D, Madjoumessi M. (2016) Spirometric Lung Function Abnormalities in HIV-Infected Subjects Naive to Antiretroviral Therapy. Am Thorac Soc. 3083.
- 25.Drummond M B, Kirk G D. (2014) HIV-associated obstructive lung diseases: insights and implications for the clinician. Lancet Respir Med. 2(7), 583-92.
- 26.Pefura-Yone E W, Balkissou A D, Kengne A P. (2016) Determinants of Restrictive Spirometric Pattern in a Sub-Saharan Urban Setting: A Cross-sectional Population-based Study. Open Respir Med J. 10, 86-95.
- 27.Kristoffersen U S, Lebech A-M, Mortensen J, Gerstoft J, Gutte H et al. (2012) Changes in lung function of HIV-infected patients: a 4·5-year follow-up study. Clin Physiol Funct Imaging. 32(4), 288-95.
- 28.Koppel K, Bratt G, Schulman S, Bylund H, Sandström E. (2002) Hypofibrinolytic State in HIV- 1-Infected Patients Treated With Protease Inhibitor-Containing Highly Active Antiretroviral Therapy. J Acquir Immune Defic Syndr. 29(5), 441-9.