MRI Study and Psychological Assessment in Children and Youth with Deviation Behaviour
Abstract
Objective
Antisocial behavior (ASB) in children and youth is public health problem in Georgia. Nevertheless, there has been no systematic study the risk factors for ASB that could counteract on ASB development. To prevent ASB development and acceleration the understanding of biological (assessment of Brain morphology using MRI) and psychological (assessment using Freiburg Personality Inventory) risk factors is critical. This was the aim of this study.
Method
The children/youth with ASB tendency (AST) were identified by the Freiburg Personality Inventory (FBI). The biological and psychosocial factors contributing to AST were evaluated using a semi-structured clinical interview. Brain anatomy and morphology was studied using magnetic resonance imaging (MRI).
Results
Children/youth with AST had significant abnormalities in most axial elements of the DSM multi-axial system but not in brain anatomy measured by MRI.
Conclusion
Early identification of ASB tendencies and a provide correlationship between specific psychiatric, medical and family stress factors will likely reduce the number of children/youth with ASB and will promote their integration into society.
Author Contributions
Academic Editor: M. Camino Escolar-Llamazares, Burgos University, Spain.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Irma Khachidze, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Antisocial behavior (ASB) in children and youth is an alarming public health problem in Georgia. The Ministry of Interior and the Supreme Court of Georgia has reported 15% an increased rate of juvenile convictions and imprisonment during the past decade (www.geostat.ge). Although early Conduct Disorder CD does not necessarily develop into criminal behaviour 1, those that commit the most severe crimes also demonstrate a wide range of CD 2. Therefore, recognizing early signs of CD, associated risk factors, and a timed intervention program are critical for preventing a child's/youth’s progression from being at-risk for developing ASB, to antisocial personality disorder, and to eventually a potential criminal 3, 4, 5.
The lack of the systematic studies of possible psychosocial factors contributing to the CD development in either youth or in adults in Georgia is problematic. A two-decade gap in CD studies between Europe and North America 6, and Georgia 7, 8, 9 can be explained by the Geo-Political situation of Georgia in the past century. Soviet ideology propagated CD as a natural product of socio-cultural evolution; it did not recognize CD as a pathological condition 10 and neglected the importance of psychology in understanding the cause of CD.. For these reasons, CD was declared an unpreventable condition which allowed Soviets to control Georgian society via Soviet legislation.
Two major risk factors, constitutional and environmental factors, contribute to CD development. Constitutional factors imply genetic/personality traits 11, 12, 13 neuroendocrine disturbances and changes in brain morphology and/or function 14, 15. Environmental factors include influences from a child’s family, school, neighbourhood, community, and society 16, 17, 18. Moreover, there is interplay between biological and psychosocial risk factors in the development and progression of antisocial and delinquent behaviour 19. Additionally, CD carries significant comorbidities with a number of psychiatric disorders such as Attention Deficit Hyperactivity Disorder (ADHD) 20, 21, major depression 22, and anxiety disorder 23, 24, 25 .This study presents the systematic study of the constitutional and environmental risk factors in children and youth with CD or AS tendency in Georgia.
Methods and Materials
Participants
This study assessed and examined 69 children/youth with an age range from 10 to 18 years old and their parents. These individuals were divided into children who aged from 10-14 years subjects, while youth were defined as those aged from 14-18 years. The subjects were recruited by a regional TV announcement seeking participants for an ongoing study on children/youth with CD. CD means children till age 18 with tendencies conduct disorder. Table 1.
Table 1. Distribution of participants based on male/female, age group (10-14 vs 14-18), High CD vs low -CD| 69 | Children Male | Children Females | Youth Males | Youth Females |
| CD-52 | High CD-15(75%) | High CD | HighCD-23(88.5%) | High CD |
| Low CD-5 (25%) | Low CD- 3 | Low CD-3 (11.5%) | Low CD-3 | |
| Controls-17 |
The rationale for recruiting subjects this way was the finding that self-report delinquency is a valid and effective method for recruiting participants in studies of CD based on ”‘effects’ of parenting reconsidered”: 26. Control subjects were recruited from the same population. All subjects were informed about the voluntary and confidential nature of the study. A written consent was given by all parents (a mother) or guardians, and assent by the kids participating in the study. The study was approved by the institutional review boards of D. Uznadze Institute of Psychology (Tbilisi, Georgia) and the Ministry of Health and Wellness of Georgia. The research was conducted in compliance with the guidelines of the Georgian Psychological Society and International Union of Psychological Sciences on “Ethical Principles of Psychologists” and “Code of Conduct”, which reflect international guidelines set by the American Psychological Association (www.apa.org).
Psychological Assessment of Participants
Children / Adolescents
All child underwent a psychological personality test, the Freiburg Personality Inventory (FPI) conducted by trained psychologists 27. FPI was conducted to identify the subjects with CD. The FPI has shown to be a valuable tool for the early identification of AST. The FPI is comprised of 98 items in the form of a questionnaire. Each item on the FPI is related to one of the seven inventory scales measuring the risk/tendency for a certain personality trait:
FPI 1. Socially Desirable Response
Replies in a manner that will be viewed favorably by others
FPI 2. Breaking the Code of Practice
Breaks the norms and rules of behavior and the values established by society
FPI 3. Addictive behavior
The readiness for addictive behaviour
FPI 4. Self-destructive behaviour
The tendency to engage in certain kinds of self-destructive acts such as both social and literal suicide i.e. self harm
FPI 5. Aggression and violence
The tendency to express violence and aggression
FPI 6. Volitional control of emotional reactions
The tendency to lack cognitive appraisal of a given situation i.e. emotional reaction without awareness
FPI 7. Delinquent Behavior
The readiness to engage in delinquent behavior.
The FPI was chosen because of its high reliability and internal consistency (Cronbach's alpha) 28, 29
The combination of FPIs scores were compared between control subjects and CD subjects. Raw values were first normalized relative to FPI and later transformed to a standard score scale 30, 31. The subjects with scores within a normal range in all FPIs were denoted as “control” subjects 32.
Otherwise, the subject was considered “at-risk” for CD. To avoid highly skewed responses in the CD group, two groups were assigned for those at risk: low CD who had abnormal scores in three or less items, and those with high CD who had four or more items.
To avoid stigmatization of the children, youth, and/or their parents, each parent was given a verbal explanation of terms such as “CD”, “low and high scores in a given psychological test”, or “questionnaires” prior to the study. Moreover, if the subject was identified as a person with, CD in the future both the subject and the parent will be offered psychotherapeutic sessions (free of charge). The training program will be comprised of elements of cognitive-behavioral 33 and Rogerian therapies34 in combination with art-therapy 35.
All subjects and their mothers underwent a semi-structured individual clinical interview by a trained psychiatrist, psychologist and neurologist. The interview was based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-R; American Psychiatric Association, 2000). The interview enabled a multi-axial assessmentwhich facilitated a comprehensive and systematic evaluation of the various risk/predictive and comorbid factors
Magnetic Resonance Imaging
Brain MRI scans were performed on a 1.5 Tesla (Philips-Intera) MRI. The MRI protocol, i.e. sequences and scanning duration, was optimized for the studied age groups. The following standard protocols were used to acquire both T1 and T2 weighted images in the axial and sagittal planes: T2 TSE in axial plane, T2 FLAIR-MV in axial plain, T1 SE in sagittal plane, T2 TSE SPIR-MV in coronal plain and T2 TSE SPIR-MV in coronal plain. The whole brain was checked for anatomical abnormalities. The regions related to antisocial behaviour 15, 16) was identified as target regions.
T2 TSE in axial plane: Twenty-two images, 6 mm slice thickness, with 1 mm gap were acquired; TE - 110 ms, TR – 4889.6 ms, FOV - 230/230 mm, matrix-384/304. The signal intensity can indicate intraparenchimal abnormalities associated with necrosis, cyst formation, vasogenic and cytotoxic oedema, inflammation, etc. The major pitfall of this protocol is that high-intensity signal areas associated with brain tissue abnormalities, adjacent to ventricles and/or subarchnoidal space can be missed due to cerebrospinal fluid (CSF) signal intensity. The same areas also present a signal hyperintensity on T2 images. To avoid possible artifacts, T2 FLAIR sequencing was run as well.
T2 FLAIR-MV in axial plain: Forty-five images, 3 mm slice thickness with 1 mm gap were acquired; TE - 140 ms, TR - 11000 ms, FOV - 219/219 mm, matrix-200/50. This sequence attenuates CSF signal and therefore provides better contrast at the interface of brain with CSF, which improves the likelihood of detecting small white-matter lesions. The MV technique was used to correct motion artifacts.
T1 SE in sagittal plane: Twenty-two images, 5 mm slice thickness with 1 mm gap were acquired; TE - 15 ms, TR – 596.2 ms, FOV - 210/210 mm, matrix - 236/188. T2 sequences can provide resolution for detection of intraparenchimal damage. Nevertheless, the increased signal intensity due to oedema on T2 images might obscure a lesion. Therefore, T1 provides better anatomical detection of an underlying lesion. It also provides high contrast between gray and white matter and is well suited for the detection of cortical lesion.
The whole brain was checked for anatomical abnormalities. The regions related to antisocial behaviour7, 8, 9 was identified as target regions (see below)
The MRI protocol contained two more sequences that also improved the image quality of midline subcortical structures (e.g., hippocampus), detection of any possible tumors (without contrast agents) and abnormal tissue related to possible acute, vasogenic alterations
T2 TSE SPIR-MV in coronal plain: Twenty-eight images, 4 mm slice thickness with a 1 mm gap; TE - 120 ms, TR - 4000 ms, FOV - 199/199 mm, matrix - 332/30;
DWI in axial plain: Forty-four images, 5 mm slice thickness with a 1 mm gap; TE - 74 ms, TR – 3206.6 ms, b-values of 500 or 1000; FOV - 229/229 mm, matrix-112/89.
The following areas were identified as target regions: frontal lobe 15, 16, 37, 38, temporal lobe 38, parietal lobe/angular gyrus and cingulate cortex 39, hippocampus 40, 41, amygdala 42, and corpus callosum 43. The abnormalities in the above mentioned structures have been reported to disrupt moral thinking and feeling, produce poor emotional decision making, behavioral planning, attentional shifts, memory disabilities, and problems in reading and arithmetic. Abnormalities in these areas can predispose and give rise to antisocial tendencies (rule-breaking) and/or behaviour 44, 45
Lesion Classification/Characterization
MRI images were evaluated using qualitative and a pseudo-quantitative assessment by neuroradiologists blind to the clinical history of the patient, diagnosis, and sequence type; the images were viewed in random order. Image artifacts (i.e. motion and flow-related artifacts) were evaluated regarding artifact influence on image interpretation on a subjective scale (0 = no artifact; 1 = mild artifact; 2 = moderate artifact; or 3 = severe artifact). If there was an image with a severe artifact the image was rejected from further analyses, three patients were rejected in the study of the 69 individuals). The location and number of lesions was assessed thereafter. The images were compared side by side to delineate the lesion from adjacent structures and to properly characterize the lesion. The images were visually inspected for focal abnormalities. Abnormalities were identified in accordance with MR semiotics based on characteristics of focal intensity. If there were major volumetric changes, crude measurements were made and then compared to age-appropriate controls.
Statistical Analysis
Statistical analysis was performed using SPSS 13. Data were treated as categorical data according to the definition by Field and Hole 35. The relation between two categorical variables was checked using the Pearson chi-square test. Category 1 was the Group Studied and Category 2 was one of the studied variables. Effect size was measured using the odds ratio. Likelihood ratio statistics were measured for the final model. High-order interactions were broken-down for follow-up analyses and chi-square analyses were conducted at different levels for each variable. In order to identify the most important effect, z-scores were calculated and compared between effects.
The effect of psychotherapy/training on children’s CD was evaluated by Wilcoxon signed-ranks test.
The “improvement” score for each age group was calculated (Δ = before “FBI score” - after “FBI score”) and compared. For all analysis p < 0.05 was considered statistically significant. The relation between two categorical variables was checked using the Pearson chi-square test. Category 1 was the Group Studied and Category 2 was one of the studied variables. Phi considered as to mild, moderate or significant
Results
Participants
Sixty-nine 10-18year-old girls and boys participated in this study Fifty-two of the subjects had CD. Only six of them were girls, small female group, not statistically significant for comparison with the control group. Among forty-six AST boys, twenty boys were 10-14 years old and twenty-six were 14-18year-old (Figure 1A). The age and severity of CD (low vs. high) were explored only for boys. No signs of CD were found in seventeen boys and they formed the control group. Details on subject demographics and FPI assessment are summarized in Figure 1B.
Figure 1.Distribution (%) of subjects with antisocial tendencies (AST) by age and level of AST in (A) studied subjects and (B) the subjects with AST only. If the subject scores were up to three Freiburg Personality Inventory (FPI) scales above the normal range, he/she was considered with low AST. Higher scores in four and more FPI scales classified the child/youth with High AST.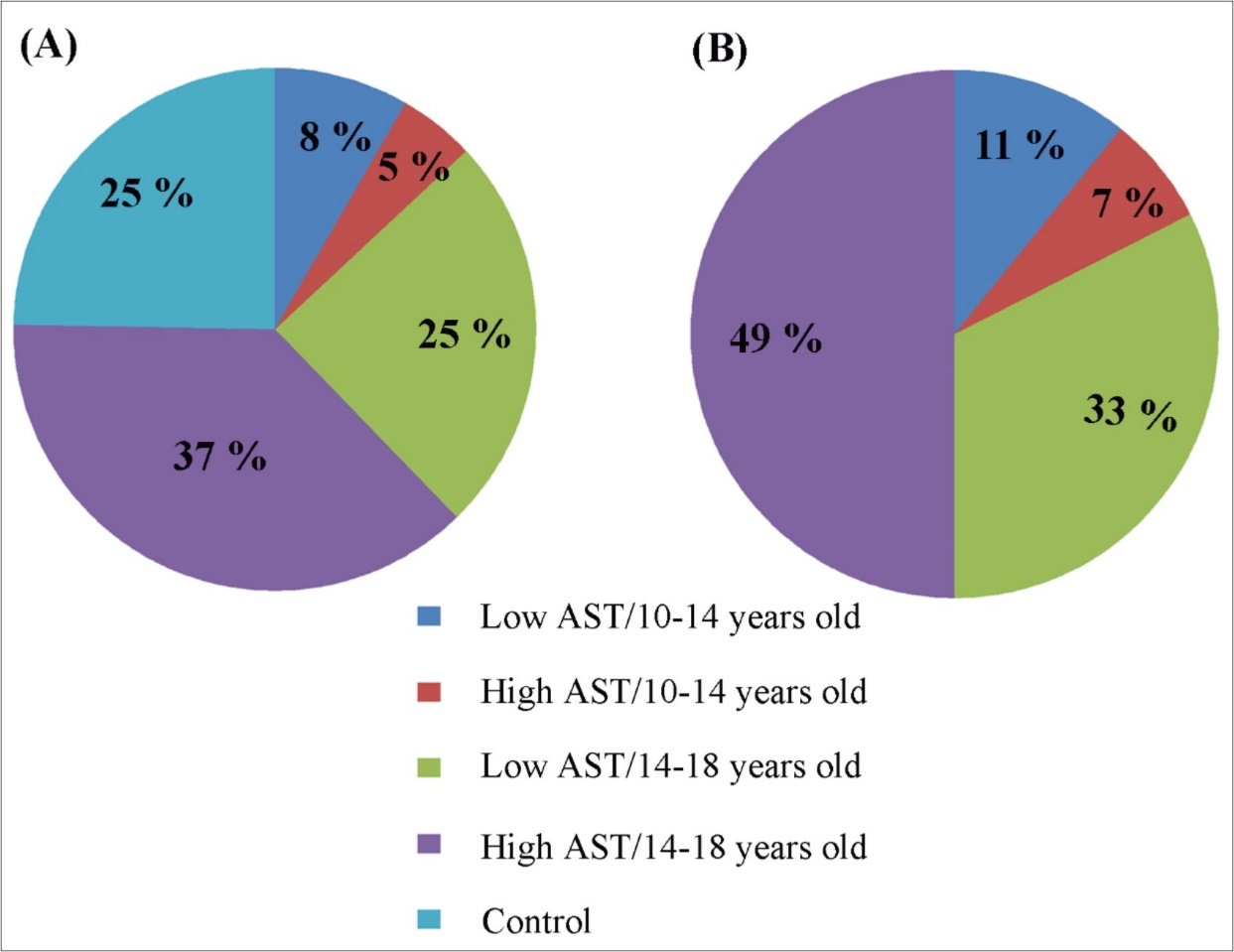
The age and severity of CD (low vs. high) were explored only for boys, because the group size for girls with CD was small, this as limitation consequently, no gender effect was evaluated. The age and severity of CD (low vs. high) were explored only for boys.
Child and Youth with CD vs. Control
Youth and children with CD revealed abnormalities in almost all axial elements of the DSM IV compared to control subjects. Aggression and academic underachievement were the strongest predictors of CD.
Axial I –Psychiatric Conditions
Children/youth with CD suffered from multiple mood disorders. Prevalence of aggression (c2 = 27.05, p < 0.001; OR = 55.7, Phi = 0.626) had the highest power to predict CD; prevalence of anxiety was 6.3 times higher in CD children/youth compared to controls (c2 = 9.6; p < 0.003; Phi = 0.379); prevalence of depression associated with CD (c2 = 9.9, p < 0.003; OR = 9.5, Phi = 0.373). However, there was no association between phobia, ADHD, or head trauma and CD(p > 0.05). Only subject with ADHD has some tendency.
Among substance related disorders, only tobacco smoking (c2 = 9.8; p < 0.003; OR = 15.3) and alcohol consumption (c2 = 6.2; p < 0.02; OR = 4.2) were significantly associated with AST. However, the strength of association was moderate (Phi=0.378) and low (Phi=0.301), respectively.
Axial II – Personality Disorders
(Figure 1) depicts the prevalence of low- and high-CD in studied subjects. Distribution (%) of subjects with CD tendencies by age and level of CD in (A) studied subjects and (B) the subjects with CD only.
Axial III – General Medical Condition
The prevalence of maternal emotional disturbances during puerperium (c2 = 16.4, p < 0.001; OR = 11.5, Phi < 0.3 ) and pregnancy (c2 = 11.2, p < 0.002; OR = 7.7; Phi < 0.3) was significantly higher in the CD group compared to controls (Phi: 0.43 – 0.49). Family conflict (c2 = 8.6, p < 0.004, Phi < 0.3) and family violence (c2 = 7.8, p < 0.006, Phi < 0.2 ) also occurred with a moderately higher prevalence (~ 7 times more) compared to the families of the control group (Phi: 0.34 – 0. 0.40). A mild but significant association was found between the father’s reaction to pregnancy and CD (c2 = 4.4, p < 0.04; OR = 15.3, Phi < 0.3 and (c2 = 6.2, p < 0.02; OR = 5.3, Phi < 0.3).
Among other medical conditions, a relatively higher prevalence asphyxia/hypoxia during birth was related to an increase in AST (c2 = 4.4, p < 0.04; OR = 5.3, Phi < 0.3). No significant association was found between epilepsy and AST (p > 0.05). Only two individuals had epilepsy, one in controls vs one with CD?
Axial IV – Psychosocial and Environmental Problems
Low academic achievement was the strongest predictor of CD among all studied psychosocial and environmental factors (c2 = 19.99, p < 0.001; OR = 19.4, Phi = 0.538). Youth that dropped out of school \ primary support group also significantly increased the prevalence of CD. Children and youth from families that ignored the child’s/youth’s inability to cope or to solve behavioural problems had a 24.2 times higher prevalence of CD (c2 = 16.6, p < 0.001; Phi = 0.49). In addition, lesser interest in a child’s/youth’s personal life increased CD 11.1 times (c2 = 11.6, p < 0.002; Phi = 0.41).
Social environment was also posed as CD risk factor. Family conflict and parental unemployment significantly increased the number of children/youth showing CD (c2 = 16.4, p < 0.001; OR = 11.5, Phi = 0.49) and (c2 = 9.15, p < 0.002; OR = 14, Phi = 0.36), respectively. Separation and divorce were among the risk factors but was only weakly correlated with CD (c2 = 5.1; p < 0.03; OR = 8.2, Phi < 0.3).
Boys with CD vs. Control
Pearson’s chi-square analyses revealed comparable comorbid and risk factors for AST when boys and girl were analyzed separately and when they analyzed together. Specifically, aggression (c2 = 24.3; p < 0.001; OR = 50.7, Phi < 0.7) and academic underachievement (c2 = 19.8; p < 0.001; OR = 25.14, Phi < 0.6) were the factors most strongly associated with CD in boys. Females are small in number in both groups and were thus not analyzed. Thus, the age and severity of CD (low vs. high) were explored only in boys.
The Effect of Age in Boys with CD vs. Control
The comorbid and risk factors of CD were comparable in boys of different ages, however break-down of the data at different levels of age by chi-square analysis revealed few age-related effects.
Aggression (c2 = 24.9; p < 0.001, Phi < 0.6), anxiety (c2 = 19; p < 0.001, Phi < 0.5), tobacco smoking (c2 = 21.4; p < 0.001, Phi < 0.6), and puerperium depression (c2 = 22.8; p < 0.001, Phi < 0.6) were strongly associated with AST at all ages. The lack of analytical tools to solve the problem (c2 = 18.1; p < 0.001, Phi < 0.5) and conflicts in the family (c2 = 16.8; p < 0.001, Phi < 0.5) also increased AST in younger and older boys.
Most importantly, significantly high prevalence of anxiety was found in 14-18 year-old boys with AST compared to 10-14 year-old boys (c2 = 11.3; p < 0.001; OR = 20.5, Phi = 0.50).
The Effect of Age in Boys with High-CD
The break-down of the data at different levels of age by chi-square analysis revealed few age-related effects. Anxiety level was 15 times higher in 14-18 year old boys compared to 10-14 year old boys (c2 = 10.93; p < 0.001; Phi = 0.54).
MRI
MR images revealed alterations in brain tissue only in boys with CD (n = 10), however there was no statistical significance between brain malformation and CD. Cerebral dysgenesis was the most prevalent brain abnormality. CD subjects displayed (Figure 2); 1. Medial temporal lobe sclerosis (hypotrophy of either right or left hippocampus) (n = 2); 2. Hypogenesis of the corpus callosum i.e. the band of white matter connecting the two hemispheres of the brain, failed to develop normally and was thinner than in healthy subjects (n = 1); 3. Gray matter heterotrophy, a type of cortical dysplasia, which results in the mislocation of neurons during neuronal migration (n = 2); 4. Arnold-Chiari malformation type II, characterized by a downward displacement of the cerebellar tonsils (hypoplastic cerebellum) through the foramen magnum (n = 1); 5.Arachnoid cysts in the temporal lobe and frontal convex (n = 2). All but two of the subjects described above had mothers with a history of stress and/or various complications during pregnancy and/or labor. Moreover, subjects with the described brain malformations showed signs of epilepsy and/or ADHD they have been excluded – in CD people. Only one subject, having corpus callosum hypogenesis and gray matter heterotrophy in the parietal lobe, showed mild neurological symptoms, having conduct disorder with intellectual disability
Figure 2.Representative images of the brain abnormalities observed in some children with the tendency of antisocial behavior (AST) by Magnetic Resonance Imaging (MRI). Coronal sections (4 mm thick) were acquired by T2 turpbo spin echo (TSE) multi vane (MV) sequence; Axial sections (6mm thick) - T2 TSE.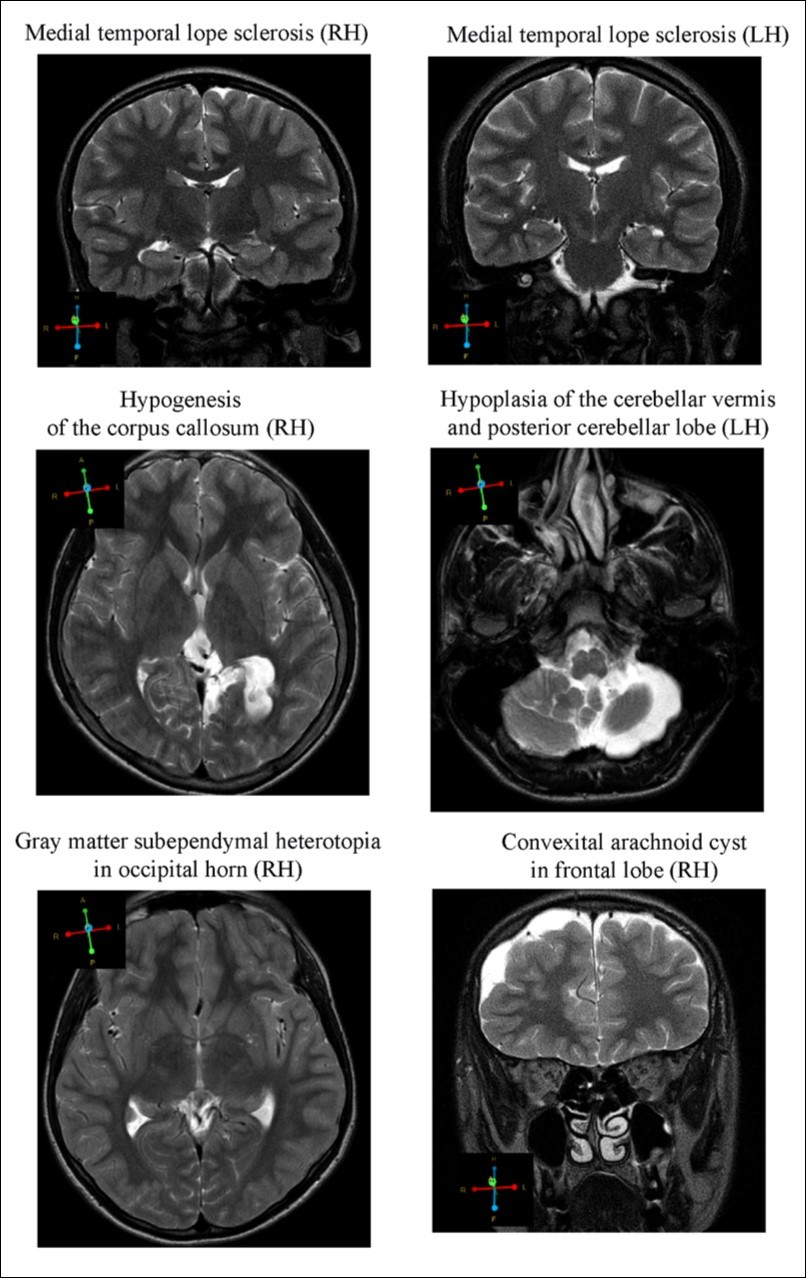
Discussion
Conduct disorder (CD) generally refers to actions that deviate significantly from established social norms. Signs of CD can be identified in children at a young age. The main approaches to identify factors contributing to the development and acceleration of ASB. Both possible biological and psychosocial risk factors for CD were assessed in order to design possible preventive strategies against CD development. In this study have not found o statistical significance between brain malformation and CD.
In principle, there are two main approaches to counteract the development and acceleration of CD. One can identify possible biological and psychosocial risk factors of AST in order to design preventive strategies against CD development. Though, the other approach is to develop an effective therapy (Stevens, 2008) for people with CD in order to offset the eventual transition of CD to enduring CD. Thus, the present study evaluated the risk and prognostic factors of CD in youth and children in Georgia. Most importantly, explored the group of children/youth with CD and in future works will provide psychotherapy and then evaluate the efficiency of to eliminate early signs of CD and to counteract CD development.
The present study yielded a high prevalence of aggression in children and youth with CD. Additionally, the measure of aggression contrasted between the boys with low- vs. high-CD. The incidence of aggression gradually increased from the low-CD to the high-CD group compared to healthy children and youth. Although aggression scores in this study are based on children and parental reports, it has a high reliability for prediction of CD 46. Thus, aggression can be considered a reliable marker for identifying the signs of CD in children and youth. Additionally, it can facilitate the identification the boys with high- vs. low-CD., The next study, the group of boys requiring a targeted intervention (e.g., psychotherapy) in order to prevent the transition from CD into permanent CD. The outcome of this study in Georgia with comparison the rest of Europe, USA and for instance, with previous studies 47, 48, would expect a cross-national similarity in the relationship pattern between aggression and CD. Also, it was expected to have behavioral issues in those with maternal depression or psychosocial stressors.
This study has been some limitations (small female group, small control group, study was depend on scales). Also, inclusion of children with neurological disorders might have biased the outcome. In future work would include female subject to avoid some of the limitations in this study.
The current study might benefit for future studies: Thus, the present study evaluated the risk and prognostic factors of CD in youth and children in Georgia. Most importantly, the group of children/youth with AST will be explored and will be evaluated the efficacy of psychotherapy to eliminate early signs of CD and to counteract CD development. In future works both the subject and the parent will be offered psychotherapeutic sessions (free of charge).
Thought it is sufficient amount for study brain morphology and Lesion classification/characterization, that is the main aim of work. For psychological assessment should be some limitation. But main goals of work was study of brain morphology in children/youth at risk of CD. A standard clinical evaluation of brain tissue by MRI did not reveal any association between brain abnormalities and CD. Although changes in cortical and subcortical regions and white matter were found in a few children with CD, the relationship was not significant. Nevertheless, brain abnormalities have previously been reported in children with CD 15, 16, 49 aggressive and violent offenders 50 psychopaths and murderers 51. In the present study, there are few reasons for a low prediction of CD by MRI. Firstly, the MRI analyses are likely not sensitive enough to capture very early stages of ASB 37. In the future it may be interesting to determine whether the measure of grey and white matter volume can predict CD. Moreover, future functional MRI or positron emission tomography (PET) studies during resting state and/or in response to cognitive and emotional tasks 52, 53 may reveal abnormalities in brain function in CD children/youth. Currently, the causal relationship between the structural/functional deficits of the brain and CD remains unclear. One can hypothesis that brain deficits cause, CD whereas others can argue that the brain abnormalities could also result from the practice of an antisocial lifestyle.
Conclusion
In conclusion, the findings of the present study indicate (i) that the risk and comorbid factors in Georgian boys with CD are similar to those found in children and youth in Europe and North America; (ii) We thought, education of a child’s psychosocial environment (e.g., mother 54, early identification of the signs of CD, offering psychotherapeutic sessions will potentially reduce the number of children/youth with CD and promote their integration to society, that is aim of our next study
Acknowledgment
We are grateful to Anti-Drug Center at the Patriarchate of all Georgia. We also would like to thank the D. Uznadze Institute of Psychology (Tbilisi, Georgia) and Child Neurology Department of Tbilisi State Medical University. The authors have no conflict of interest to declare.
Abbreviations
References
- 1.Remschmidt H, Walter R. (2010) The long-term outcome of delinquent children: a 30-year follow-up study.Biological Child and Adolescent Psychiatry, J Neural Transm. responsible children.New York, NY:Three Rivers Press. 117, 663-677.
- 2.Ruchkin V, Koposov R, Eisemann M, Hagglof B. (2001) Conduct problems in Russian adolesents: the role of personality and parental rearing,European. , Child & Adolescent Psychiatry 10, 19-27.
- 3.Sh Li, Karatzoglou A, Gentile C. (2016) Collaborative Filtering Bandits. Proceedings of the 39th International ACM SIGIR conference on Research and Development in Information Retrieval, SIGIR , Pisa, Italy 539-548.
- 4.Li. (2016) The Art of Clustering Bandits", the University of Oxford. IEEE International conference on Ubiquitous Intelligence and Computing, Università degli Studi dell' Insubria, Dissertation, Seoul, Korea , Oxford, UK 216-223.
- 5.Harasymiuk J, Szafranko H, Tyburski J. (2019) Methods of habitat reports’ evaluation https://doi.org/10.1515/eng-2019-0001. , Journal of Engineering 9, 26-33.
- 6.J F Christopher. (2010) Genetic Contributions to Antisocial Personality and Behavior: A Meta-Analytic Review From an Evolutionary Perspective,The. , Journalof Social 150(2), 160-180.
- 8.Gabiani A, R G Gachechiladze. (1982) The geography of criminal behavior, based on criminal evidence inGeorgian SSR. , Tbilisi:TbilisiStateUniversity 143.
- 10.J I Gilinsky.(2003).Sociology of a deviant behavior and a social control. Sociology of deviant behavior and social control. In: Sociology in. , Russia 22, 587-609.
- 11.Foley L, Eaves L, Wormaly B, Silberg J, Maes H et al. (2004) Childhood adversity, Monoamine Oxidase A genotype, and risk for conduct disorder. ArchGen Psychiatry61:. 738-744.
- 12.Scott S, Knapp M, Henderson J, Maughan B. (2001) Financial cost of social exclusion: Follow up study of antisocial children into adulthood. , British Medical Journal 323, 191-194.
- 13.Scourfield J, Bree M Van den, McGuffin M. (2004) Conduct problems in children and adolescents: A twin study. Archives of General Psychiatry,61 489-449.
- 14.Kruesi P, Manuel F, Mannheim G, Johnson-Bilder A. (2004) Reduced temporal lobe volume in early onset conduct disorder,MedicalUniversityof SouthCarolina,1-11.
- 15.Raine A, Yang Y. (2006) The neuroanatomical bases of psychopathy: a review of brain imaging findings. In: Patrick C.J. (ed),Handbook of Psychopathy.GuilfordPress,278-295.New York.
- 16.Reid J, Patterson G, Snyder J. (2002) Antisocial behavior in children and adolescents: A developmental analysis and model for interevention. , Washington, DC:AmericanPsychological Association,724-725
- 17.Loeber R, Farrington P. (2000) Young children who commit crime: epidemiology, developmental origins, risk factors, early interventions, and policy implications.Development and Psychopathology2000;. 12, 737-762.
- 18.D P Farrington. (2003) What Has Been Learned from Self Reports about Criminal Careers and the Causes of Offending? London: Home Office. , Research Findings 281.
- 19.Holmes E, Saughter R, Kashani J. (2001) Risk. factors in childhood that lead to the developmental of conduct disorder and antisocial personality disorder.PsychaitHum Dev;. 31, 183-93.
- 20.Farrington D, Loeber R, W Van Kammen. (1990) Long-term criminal outcomes of hyperactivity, impulsivity, attention deficit and conduct problems in childhood.Straight and devious pathways from childhood to adulthood. , Cambridge, England:CambridgeUniversityPress 19, 62-81.
- 21.Klein R, Mannuzza S. (1991) Long-term outcome of hyperactive children:. A review.Journal of the AmericanAcademy of Child and Adolescent Psychiatry,30 383-387.
- 22.Righetti-Veltema M, Conne-Perreard E, Bousquet A, Manzano J. (2002) Postpartum depression and mother-infant relationship at 3 months old.Journal of Affective Disorders. 70, 291-306.
- 23.Angold A, Costello J, Erkanli A. (1999) . , Comorbidity.Journal of Child Psychology and Psychiatry 40(1), 57-87.
- 24.Pliszka R, Liotti M, Woldorf M. (2000) Inhibitory control in children with attention-deficit/hyperactivity disorder: Eventrelated potentials identify the processing component and timing of an impaired right-frontal response-inhibitionmechanism.Biological. , Psychiatry 48, 238-246.
- 25.Vermeiren R, Deboutte D, Ruchkin V, Schwab-Stone M. (2002) . Antisocial behaviour and mental health. Findings from three communities.European Child & Adolescent Psychiatry,11: 168-175.
- 26.T G O'Connor. (2002) Annotation: The ‘effects’ of parenting reconsidered: findings, challenges. , and applications.Journal of Child Psychology and Psychiatry 43, 555-572.
- 27.Fahrenberg J, Selg H, Hampel R. (1970) Das Freiburger Persönlichkeitsinventar (FPI). , Göttingen: Hogrefe
- 28.J M Bland, D G Altman. (1997) . Statistics notes: Cronbach's alpha.British MedicalJournal,314: 572.
- 29.R J Shavelson. (2004) Editor’s preface to Lee J. Cronbach’s ‘‘My Current Thoughts. on Coefficient Alpha and Successor Procedures.’’Educational & Psychological Measurement 64(3), 389-390.
- 30.N P Fetinski, V, G M Manuilov. (2002) Social-psychological diagnostic of small groups.Book of the institute of psychotherapy. 490.
- 31.U A Kleiberg. (2004) Social-psychological problems of deviant adolescents,Monograph. , Strasburg, Moscow,148
- 32.Fahrenberg J, Johannes B. (2009) Ebner- structural MRI studies in personality Priemer, U. Ambulatory activity monitoring: Progress in measurement of activity, posture, and specific motion patterns in daily life. , European Psychologist 14(2), 142-152.
- 33.Aaron T Beck. (1975) . Cognitive Therapy and the Emotional Disorders.InternationalUniversitiesPressInc 0-8236.
- 34.Rogers C. (1957) The necessary and sufficient conditions of therapeutic personality change’. , Journal of Consulting Psychology 21(2), 95-103.
- 36.Raine A, Yang Y. (2011) Quitting Behaviour in the Australian Population: Evidence from. , National Cross-Sectional Surveys.AustN Z 45(2), 170-178.
- 37.Laakso M, Gunning-Dixon F, Vaurio O, Repo-Tiihonen E, Soininen H et al. (2002) Prefrontal volumes in habitually violent subjects with antisocial personality disorder and type 2 alcoholism.Psychiatry Research,114:. 95-102.
- 38.M C Dolan, J F Deakin, Roberts N, I M Anderson. (2002) Quantitative frontal and temporal -disordered offenders and control subjects. , Psychiatry Research 116, 133-149.
- 39.Wong M, Lumsden J, Fenton G, Fenwick P. (1997) . Neuroimaging in mentally abnormal offenders.Issues Criminology and Legal Psychology 27, 49-58.
- 40.Raine A, Ishikawa S, Arce E, Lencz T, Knuth H et al. (2004) Hippocampal structural asymmetry in unsuccessful psychopaths.Biological. Psychiatry,55: 185-191.
- 41.Yang S, Glenn B, Raine D. (2008) . Brain Abnormalities in Antisocial Individuals:Implications for the Law 65-80.
- 42.Tiihonen J, Hodgins S, Vaurio O. (2000) Amygdaloid volume loss in psychopathy. Society for Neuroscience Abstracts,2017. Revision received May15,2002.Accepted.
- 43.Raine A, Phil D, Lencz T, Taylor K, Hellige J et al. (2003) . Corpus Callosum Abnormalities in Psychopathic Antisocial Individuals,ArchGen Psychiatry,60(11): 1134-1142.
- 44.Raine A. (2006) The neuroanatomical bases of psychopathy: a review of brain imaging findings. In: Patrick C.J. (ed),Handbook of Psychopathy. , New York,pp 278-295.
- 45.Harasymiuk J, Szafranko H, Tyburski J. (2019) Methods of habitat reports’ evaluation https://doi.org/10.1515/eng-2019-0001. , Journal of Engineering 9, 26-33.
- 46.M J Stevens. (2008) Professional ethics in multicultural and international context. In UP. Gielen JG. Draguns, JM. Fish(Eds.), Mahwah, NJ: Erlbaum.Principles of multiculturalcounselingand therapy,31: 135-166.
- 47.Giunta D, Pastorelli C, Eisenberg N, Gerbino M, Castellani V et al. (2010) Developmental trajectories of physical aggression: prediction of overt and covert antisocial behaviors from self- and mothers’ reports. , Eur ChildAdolescPsychiatry 19, 873-882.
- 48.Giunta D, Deater-Deckard K, Lansford E, Malone P, Alampay L. (2010) The association between parental warmth and control in thirteen cultural groups.Journal of Family Psychology. 25(5), 790-4.
- 49.Manes F, Sahakian B, Clark L, Rogers R, Antoun N et al. (2002) Decision-making processes following damageto the prefrontal cortex. Brain,125: 624-639.
- 50.Damasio R, Tranel D, Damasio H. (1990) Individuals with sociopathic behavior caused by frontal damage fail to respond autonomically to social stimuli.BehavBrain Res41:. 81-94.
- 52.A L Glenn, Raine A. (2011) Antisocial Personality Disorders. , In J Decety, J Cacioppo(Eds).The Oxford Handbook of Social Neuroscience,New York:OxfordUniversityPress 885-894.
