Hirsutism and Anthropometric Profiles Among Subjects with Polycystic Ovarian Morphology? A Cross-Sectional Analysis
Abstract
Background
Polycystic ovarian syndrome (PCOS) is increasingly being diagnosed and treated with sometimes variable lifestyle advice and pharmacological interventions. Obesity is considered as the sole culprit and variable definitions in clinics compound the understanding of pathogenic heterogeneity of this syndrome. We evaluated the differences between various simple to calculate anthropometric indices along with some anthropometric-biochemical equations in subjects with or without PCOS.
Objective
To compare traditional measures like waist to hip and height ratio (WHpR and WHtR), BMI, newer markers depicting central obesity like Abdominal Volume index(AVI), Body roundness index (BRI), A Body Shape index (ABSI), Conicity index (C-index) along with biochemical-anthropometric equations like lipid Accumulation Products (LAP), Visceral Adiposity Index (VAI) and Chinese Visceral Adiposity Index (CVAI) for diagnosing PCOS as per the Rotterdam criteria
Design
Cross-sectional analysis
Place & Study Duration
Naval hospital, Islamabad from Jan- 2018 to July- 2019
Subjects and Methods
From our finally evaluated 333 female subjects we initially compared the differences for the presence of hirsutism as per modified Ferrimen Gallwey scores and biochemical hyperandrogenism by measuring free androgen index (Total testosterone/SHBG x 1000. We evaluated waist circumference, BMI, WHpR, WHtR,AVI, BRI, ABSI, C-index along with biochemical-anthropometric equations like LAP, VAI and CVAI for differences in subjects diagnosed to have PCOS by Rotterdam criteria or ultrasonography alone.
Results
Differences in hirsutism as defined by modified FG score between subjects defined to have PCOS or otherwise as per Rotterdam defined criteria were as [(PCOS=169, Mean=17.33 + 9.05) (No PCOS=164, Mean=8.21 + 5.74), p< 0.001] and ultrasound [(PCOS=87, Mean=16.95 + 9.57) (No PCOS=246, Mean=11.38 + 8.51), p< 0.001]. Similarly, the differences in FAI between subjects defined to have PCOS or otherwise as per Rotterdam criteria and ultrasound were as [(PCOS=169, Mean=6.41 + 4.88) (No PCOS=164, Mean=2.77 + 1.79), p< 0.001] and [(PCOS=87, Mean=5.75 + 5.01) (No PCOS=246, Mean=4.22 + 3.68), p= 0.011]. Anthropometric measures and anthropometric-mathematical equations were raised in non-PCOS subjects than PCOS subjects. Lean-PCOS demonstrated lower degree of hirsutism and biochemical hyperandrogenism in comparison to obese-PCOS.
Conclusion
Hirsutism and free androgen indices were raised in PCOS females. Anthropometric based measurements were not different in PCOS cases and non-PCOS females. Lean-PCOS demonstrated lower degree of hirsutism and biochemical hyperandrogenism in comparison to obese-PCOS.
Author Contributions
Academic Editor: Qianqian Song, Wake Forest School of Medicine, Wake Forest Baptist Comprehensive Cancer Center, Medical Center Boulevard, Winston-Salem, NC 27157, United States.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2019 Sikandar Hayat Khan, et al.
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Polycystic ovarian morphology or Polycystic ovarian syndrome (PCOS), termed in common parlance as the “The thief of womanhood” has emerged in recent times as a spectrum of disorders starting from menorrhagia, hirsutism to infertility. 1 The disorder not just carries with it the stigmata of reproductive disorders but also linked with various metabolic risks including insulin resistance and dyslipidemia.2 Though not much appreciated in developing countries, the problem is growing at an alarming pace within sub-continental community with prevalence touching up to 9% of the population in young females. 3
Literature review provides variable results in terms of PCOS association with clinical and metabolic risk factors. Firstly, researchers have discovered different phenotypes of PCOS as regards to their clinic-pathological correlates, which vary as per the geographical zone one belongs to. 4The usual diagnosis revolves around establishing not just the clinical presentation including disturbances in a menstrual cycle like oligo or anovulation, but reliance has been placed on various biochemical, endocrine parameters and radiological findings for labeling subjects with PCOS. 5 Secondly, there is data to support that available evidence is suggestive of inconsistent data regarding biochemical and endocrine parameters, probably due to inherent imprecision related to analytical techniques or rapidly changing hormonal cycle within the females. 6 Finally, multiple criteria starting from NIH from 1992, to Rotterdam and AE-PCOS are available to define PCOS, but yet consensus among authorities in far from converging to a common solution. 7, 4, 8 Furthermore, local data apart from its scarcity, still has been able to identify differences in phenotype especially for the sub-continental population. 9 While the clinical presentations due to symptoms vary across the cultures, authorities in past have been suggesting a simpler way to diagnose or suspect PCOS, where the role of anthropometric measurements can play a major role especially in resource- scarce countries. 10 Earlier studies in this Pazderska et al have indirectly shown waist circumference to predict cardiometabolic disease in subjects with PCOS thus highlighting the usefulness of anthropometry in this condition. 11 Another Chinese study by Huang et al identified anthropometric indices and lipid peroxidation products to be useful in identifying the underlying risk in PCOS. 12Techatraisak et al have identified visceral adiposity index and other related measures like BMI to have the potential of predicting PCOS. 13 In recent times we had several new anthropometry based indices along with conventional parameters and anthropometric measures and biochemical mathematical equations which we as author feel can potential our diagnostic tool s to predict one of the commonest disorders affecting female fertility and onward a source to cardiometabolic risk.
In the backdrop of shared evidence regarding anthropometric measures as candidate surrogate markers for diagnosing PCOS, cost-effectiveness in relation to developing and under-developed worlds and emergence of some new anthropometric measures with probable higher yields we decided to carry out a study to see the utility of various anthropometric measures and PCOS. The objective will be to compare traditional measures like waist to hip and height ratio (WHpR and WHtR), BMI, newer markers depicting central obesity like visceral adiposity index(VAI), Abdominal Volume index(AVI), Body roundness index (BRI), A Body Shape Index (ABSI), Conicity index (C-index) along with biochemical-anthropometric equations like lipid peroxidation for diagnosing PCOS as per the Rotterdam criteria.
Subjects and Methods
This cross-sectional survey was conducted at the department of gynecology & obstetrics, pathology and Radiology departments of Naval Hospital Islamabad from Jan-2018 to July-2019. The project “PCOS study” has the formal approval of “Hospital’s ethical review committee” who monitored the study throughout its course of conduct. Final signed “Ethical approval letter” was issued at the end of the study. The target population was non - pregnant female subjects who presented at the department of gynecology or female out-patient departments with history of menstrual disturbances. Subjects who had history of any chronic disease process like autoimmune disorder, metabolic ailments on medication like diabetes, hypertension, heart disease, presenting within two years of menarche, using oral contraceptive in the last 6 months, or had any hormonal fertility treatment and acute or chronic infectious disease process were excluded from the study. They were requested to participate in the study by coming to department of pathology in “exact medical fasting status” during 2nd day of follicular phase of their menstrual cycle. On the day of arrival at pathology department the ladies were explained about the study requirements, testing to be done and consequences of the study along with confidentiality of data. A total of 333 ladies consented by signing a written consent form, which was followed by a questionnaire- based interview. After interview, clinical examination was carried out for any signs of chronic disease, anthropometric measurements 14, degree of hirsutism as measured by modified Feriman- Gallwey score(mFG score) 15 and Free Androgen Index (FAI) by Total testosterone/SHBG x 100. Calculations were some new anthropometric measures including Abdominal Volume index (AVI), Body Roundness Index(BRI), A Body Shape Index (ABSI), Body Adiposity Index (BAI) and Conicity index(C-Index) were also done a per the given criteria. 16, 17, 18, 19, 20 Visceral Adiposity Index (VAI), Chinese Visceral Adiposity Index (CVAI) and Lipid Accumulation Products (LAP) were measured using as per standard criteria. 12, 13
10 ml blood was collected for measuring for various biochemical and endocrine parameters. After sampling patient went for radiological examination. PCOS was defined as per Rotterdam-define PCOS criteria. 12 Fasting plasma glucose, triglyceride and total cholesterol was measured by using GPO-PAP, GOD-PAP CHOD-PAP methods on Random Access Clinical Chemistry analyzer (Selecta Prom). LDLc and HDLc were measured direct enzymatic method where selective end-point method detergent and accelerator by using Merck Kit on Selecta Prom. Endocrine parameters including total testosterone and sex-hormone- binding globulin (SHBG) were analyzed on Chemiluminescent Microparticle Immunoassay (CMIA) on “ARCHITECT iSystem , Abbot Diagnostics”.
Subjects who failed to follow up for various reasons (n=23) including not turning for on given menstrual cycle date, non-medical fasting status, or needing a sample repetition and not but not returning for testing or did not undergo ultrasonography due to any reason were finally excluded from study.
Statistical Analysis
All data from Excel Microsoft program was shifted to SPSS-VERSION 24. Descriptive statistics for data including age, presence of hirsutism, anovulation, PCOS as defined by ultrasongraphy and Rotterdam criteria were calculated for mean + SD and frequency by using SPSS descriptive function. mFG scores were compared between Rotterdam defined PCOS definition and radiological presence or absence of PCOS by using independent sample t-test without using presumption of equal variances. Differences in conventional anthropometric indices, newer anthropometric indices and biochemical-anthropometric equations for presence of or absence PCOS were calculated using independent sample t-test without using presumption of equal variances.
Results
Mean age among our subjects was 27.89 (+ 7.62) years. Out of 333 subjects 93 were unmarried, while 238 subjects were married. History of anovulation was given by 205 patients while rest (n=128) did not give any menstrual cycle abnormality. Modified FG score was higher than or equal to 8 among 157 subjects in comparison to 175 ladies with less than 8 score out of the total designated 36 marks. 87 subjects were having radiological proven signs of PCOS, while 246 females did not show criteria defined PCOS signs in ovaries for PCOS. 169 females were diagnosed to have PCOS as per Rotterdam criteria against 164 who could not fulfill the criteria for PCOS. Hirsutism was found to be more prevalent in both subjects diagnosed to have PCOS either as per Rotterdam defined criteria or on ultrasonography. Figure 1 and Figure 2 Similarly free androgen index (FAI) was found to be raised in subjects with PCOS either defined by Rotterdam criteria or ultrasonography. Figure 3 and Figure 4 Lean PCOS demonstrated lower degree of hirsutism and biochemical hyperandrogenism in comparison to obese PCOS as depicted in Table 1, Table 2, Table 3, Table 4.
Figure 1.Differences in hirsutism as defined by modified FG score between subjects defined to have PCOS or otherwise as per Rotterdam defined criteria ((PCOS=169, Mean=17.33 + 9.05) (No PCOS=164, Mean=8.21 + 5.74), p< 0.001)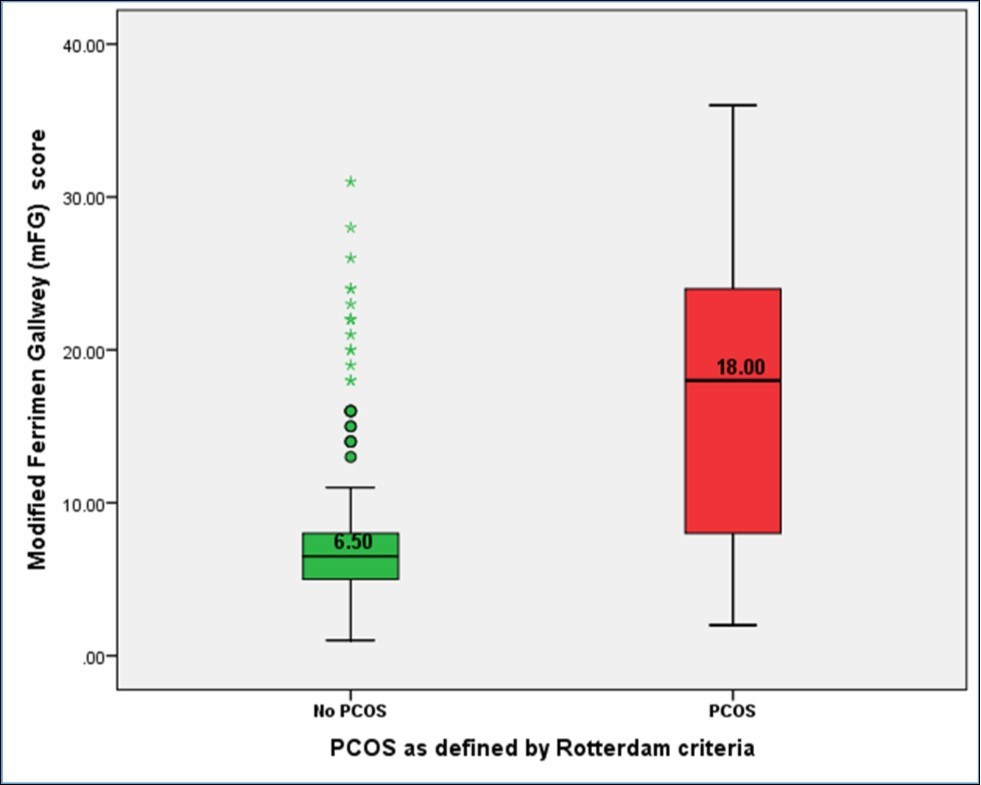
Figure 2.Differences in hirsutism as defined by modified FG score between subjects defined to have PCOS or otherwise as ultrasound diagnosis ((PCOS=87, Mean=16.95 + 9.57) (No PCOS=246, Mean=11.38 + 8.51), p< 0.001)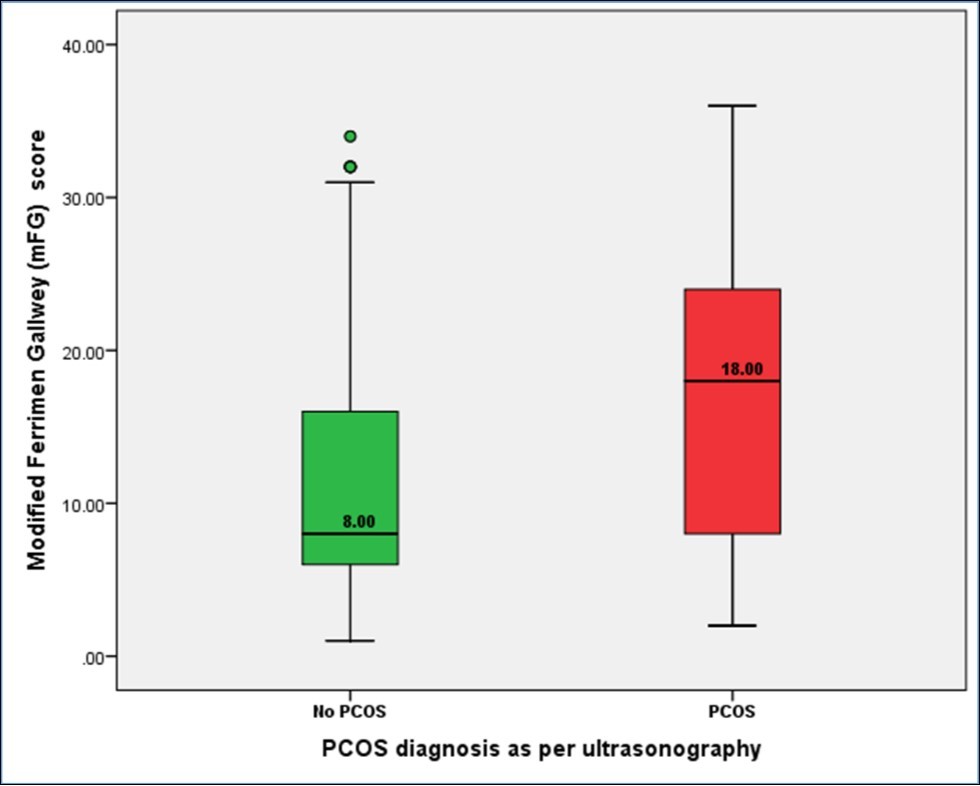
Figure 3.Differences in free androgen index (FAI) between subjects defined to have PCOS or otherwise as per Rotterdam criteria ((PCOS=169, Mean=6.41 + 4.88) (No PCOS=164, Mean=2.77 + 1.79), p< 0.001)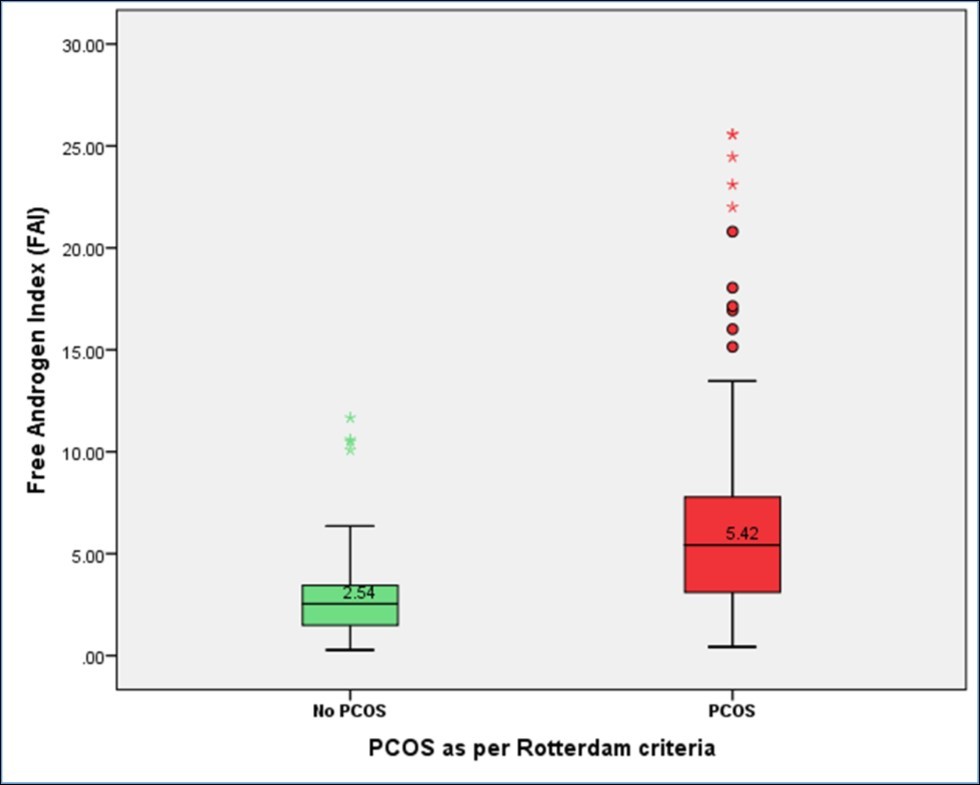
Figure 4.Differences in free androgen index (FAI) between subjects defined to have PCOS or otherwise as ultrasound diagnosis ((PCOS=87, Mean=5.75 + 5.01) (No PCOS=246, Mean=4.22 + 3.68), p= 0.011)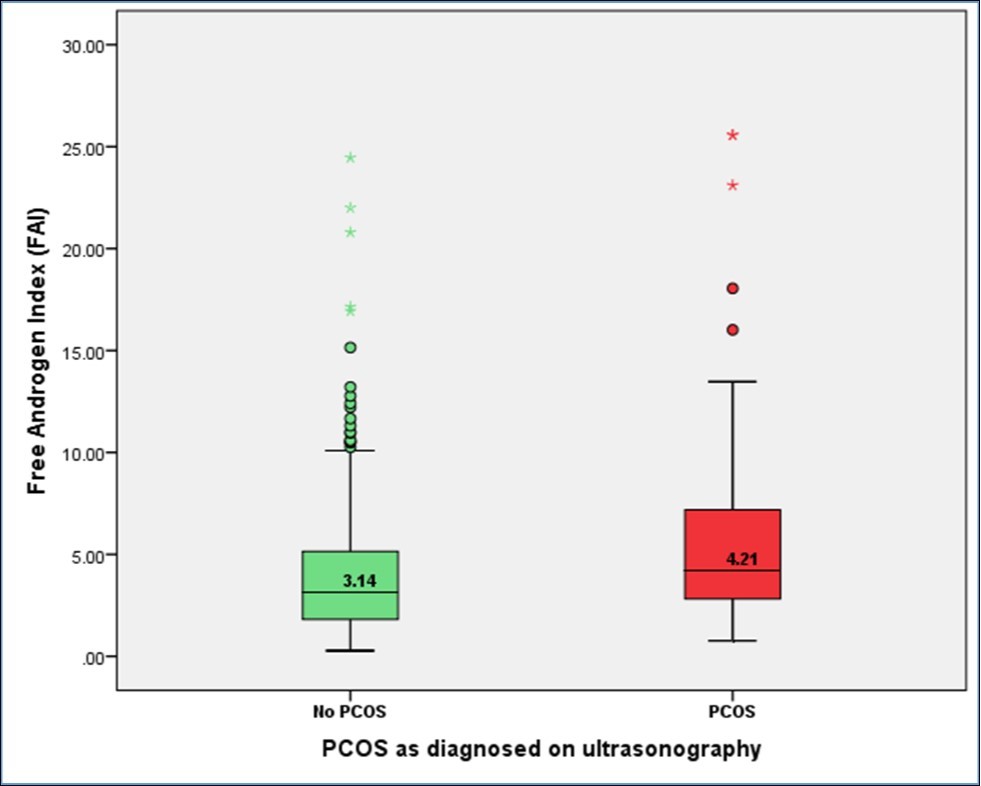
| Anthropometric measure | PCOS diagnosis (Rotterdam criteria) | Mean | Std. Dev | Sig.(2-tailed) | PCOS diagnosis (USG diagnosis) | Mean | Std. Dev | Sig.(2-tailed) |
| Waist circumference (cm) | YES (n=169) | 90.90 | 11.51 | 0.561 | YES (n=87) | 88.33 | 10.04 | 0.032 |
| NO(n=164) | 90.19 | 10.95 | NO(n=246) | 91.34 | 11.54 | |||
| BMI | YES (n=169) | 29.23 | 5.75 | 0.233 | YES (n=87) | 27.93 | 5.39 | 0.077 |
| NO(n=164) | 28.48 | 5.66 | NO(n=246) | 29.19 | 5.74 | |||
| WHpR | YES (n=169) | 0.91 | 0.054 | 0.617 | YES (n=87) | 0.903 | 0.050 | 0.098 |
| NO(n=164) | 0.91 | 0.050 | NO(n=246) | 0.913 | 0.051 | |||
| WHtR | YES (n=169) | 0.58 | 0.074 | 0.674 | YES (n=87) | 0.565 | 0.069 | 0.013 |
| NO(n=164) | 0.58 | 0.072 | NO(n=246) | 0.588 | 0.074 |
| Anthropometric measure | PCOS diagnosis (Rotterdam criteria) | Mean | Std. Dev | Sig.(2-tailed) | PCOS diagnosis (USG diagnosis) | Mean | Std. Dev | Sig.(2-tailed) |
| AVI | YES (n=169) | 16.73 | 4.14 | 0.617 | YES (n=87) | 15.81 | 3.53 | 0.029 |
| NO(n=164) | 16.50 | 3.98 | NO(n=246) | 16.91 | 4.20 | |||
| BRI | YES (n=169) | 5.75 | 5.75 | 0.621 | YES (n=87) | 5.48 | 0.94 | 0.007 |
| NO(n=164) | 5.70 | 5.66 | NO(n=246) | 5.71 | 1.00 | |||
| BAI | YES (n=169) | 33.55 | 6.04 | 0.389 | YES (n=87) | 32.13 | 5.99 | 0.034 |
| NO(n=164) | 32.99 | 5.71 | NO(n=246) | 33.69 | 5.79 | |||
| ABSI | YES (n=169) | 1.46 | 0.57 | 0.189 | YES (n=87) | 1.56 | 0.63 | 0.334 |
| NO(n=164) | 1.55 | 0.67 | NO(n=246) | 1.48 | 0.62 | |||
| Conicity index | YES (n=169) | 1.24 | 0.11 | 0.454 | YES (n=87) | 1.23 | 0.10 | 0.181 |
| NO(n=164) | 1.26 | 0.13 | NO(n=246) | 1.25 | 0.12 |
| Anthropometric measure | PCOS diagnosis (Rotterdam criteria) | Mean | Std. Dev | Sig.(2-tailed) | PCOS diagnosis (USG diagnosis) | Mean | Std. Dev | Sig.(2-tailed) |
| VAI | YES (n=169) | 0.96 | 0.09 | 0.330 | YES (n=87) | 0.95 | 0.097 | 0.330 |
| NO(n=164) | 0.97 | 0.10 | NO(n=246) | 0.97 | 0.104 | |||
| LAP | YES (n=169) | 45.88 | 34.99 | 0.839 | YES (n=87) | 45.69 | 36.31 | 0.839 |
| NO(n=164) | 45.66 | 34.76 | NO(n=246) | 46.46 | 34.31 | |||
| CVAI | YES (n=169) | 73.81 | 46.33 | 0.876 | YES (n=87) | 64.32 | 0.05034 | 0.875 |
| NO(n=164) | 74.59 | 44.74 | NO(n=246) | 76.69 | 0.051 |
| Lean or obese PCOS phenotype | N | Mean | Std. Dev | Sig. (2-tailed)* | |
| Free Androgen Index (FAI) | Obese PCOS | 120 | 6.84 | 4.83 | 0.090 |
| Lean PCOS | 48 | 5.43 | 4.92 | ||
| Modified Ferrimen Gallwey (mFG) score | Obese PCOS | 120 | 17.83 | 8.8 | 0.345 |
| Lean PCOS | 48 | 16.38 | 9.33 |
Discussion
Our findings suggested that PCOS females demonstrated higher degree of clinical hyperandrogenism as measured by hirsutism and biochemical hyperandrogenism (Free Androgen Index) among patients diagnosed to have PCOS either by Rotterdam criteria or ultrasound alone. These findings are in accordance with multiple studies on PubMed. 21, 22, 23 However, anthropometric measures including conventional, newer and mathematical models of biochemical and anthropometric measures did not demonstrated less rise in anthropometric measures among PCOS females than non-PCOS subjects especially for waist circumference, WHtR, BAI, BRI and AVI where the results were statistical significant. Lean PCOS females demonstrated slightly lower clinical and biochemical hyperandrogenism than obese PCOS subjects. This phenomena was in contrast to common belief that PCOS results due to extra fat accumulation or in some way associated with obesity as demonstrated in some studies. 24
So the First Question Arises that why Anthropometric Measures Failed to Predict PCOS?
First of all such findings have previously been defined in the literature. Gonzalez et al have suggested two types of PCOS phenotypes including lean and obese phenotype with association linked to ingestion of saturated fat diets leading to production of reactive oxygen species involved in pathogenesis of PCOS. 25 Second explanation comes in from our inclusion of females in pubertal age group, where evidence not only showing marked heterogeneity in diagnosis also provides a linking explanation where Witchel et al and Sritzer et al have suggested that pubertal developmental stage could have some overlapping features resembling PCOS and thereby suggested that the PCOS diagnosis may only be made after 2 years of menarche. 26, 27 Provided, we only included females who had at least two years of menarche, still we believe some younger females could have puberty related varying hormonal changes and the current screening recommendations may suggest a period of four or more years of after onset of menarche to allow hormonal stability. More so our sample size had only 16 females with age less than 16 years. Finally, the obesity pattern across globe varies as is true for the population from sub-continent. 7 Our study has many cases with normal anthropometric measures i.e., lean PCOS, where you may find some of the characteristics features of PCOS like oligo-ovulation/anovulation, hirsutism or biochemical hyperandrogenism as well as ultrasound evidence of PCOS but some regional data has suggested unlike the Caucasian population. Probable reason to these differences could be the specific Asian PCOS phenotype, varying environmental triggers and adipocyte behavior which have been documented to be different from non-Asian population. 28, 3, 29 Finally, Panidis et al categorized PCOS into four phenotypes where one of the phenotype with hyperandrogenism and ultrsound presence of PCOS was not associated with obesity in all phenotypes. 30
Though a long study with so many variables well-evaluated we still feel the study has limitations. Firstly, the study was a cross-sectional study which provides level-III evidence and needs to be replicated in well-controlled prospective trails. Secondly, the study was based in hospital and included mostly subjects with some clinical symptoms. Therefore, a broad spectrum epidemiological study must follow to learn the real heterogeneity and phenotypic differences within our population in order to dissect out sub-types of PCOS. We tried but also feel lack of basic education and cultural limitations could be another reason for female subjects to give clear narrative of their reproductive complaints. We will appreciate readers to interpret our findings in the backdrop of these limitations.
Clinical implications pertaining to non-significant anthropometric measures with a sizeable proportion of PCOS being lean highlights the importance of appreciating PCOS phenotypes within a given population. The evidence merits more attention as current debate suggests a different management strategy for lean PCOS types then obese PCOS patients. 31 We also want to highlight the heterogeneity of PCOS in terms of underlying pathogenesis as being multifactorial in origin, and may actually depict different metabolic pathways converging to common symptomatology.
Conclusion
Though Rotterdam defined PCOS criteria and radiological diagnosis of PCOS had significantly higher scores for clinical (modified FG cores for hirsutism) and biochemical hyperandrogenism (Free Androgen Index), still anthropometric measures the anthropometric measures or anthropometry couple biochemical equations did not show higher obesity indices among subjects with PCOS as per Rotterdam defined criteria indicating a lean-PCOS pattern in our studied population.
Declarations
Ethical approval - The project “Hyperandrogenism, hirsutism and anthropometric profiles among subjects with polycystic ovarian morphology? A cross-sectional analysis” was approved by ethical review committee of the hospital. All participants signed “Informed Written Consent Performa” and were explained about the study project.
Data Output Availability
SPSS data outputs are available from corresponding author, if demanded.
Author’s Contributions
SHK: (Corresponding author) Idea conception, Study plan, laboratory testing, result analysis, manuscript writing.
AAG: History writing, data analysis, medical writing.
RM: Study plan, sampling of subjects, statistical review and manuscript writing.
AHB: History, data analysis and manuscript help and contributed discussion.
RA: History writing, examination, medical writing
TC: Study plan, statistical review medical writing. All authors approved the final manuscript.
Consent for Publication
We got written consent and signs from all participants.
Data Funding
The study had no funding source to disclose.
Acknowledgements
The authors acknowledge the work of Lab technician Ibrahim, Miss Huma and Lab technician Iftikhar for the support and help.
Abbreviations
Body Roundness Index (BRI)
References
- 1.Moghetti P, Carmina E, V De Leo, Lanzone A, Orio F et al. (2015) How to manage the reproductive issues of PCOS: a 2015 integrated endocrinological and gynecological consensus statement of the Italian Society of Endocrinology. J Endocrinol Invest. 38(9), 1025-37.
- 2.Majid H, Masood Q, Khan A H. (2017) Homeostatic Model Assessment for Insulin Resistance (HOMA-IR): A Better Marker for Evaluating Insulin Resistance than Fasting Insulin in Women with Polycystic Ovarian Syndrome. J Coll Physicians Surg Pak. 27(3), 123-126.
- 3.Nidhi R, Padmalatha V, Nagarathna R, Amritanshu R. (2011) Prevalence of polycystic ovarian syndrome in Indian adolescents. J Pediatr Adolesc Gynecol. 24(4), 223-7.
- 4.Bozdag G, Mumusoglu S, Zengin D, Karabulut E, Yildiz B O. (2016) The prevalence and phenotypic features of polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod. 31(12), 2841-2855.
- 5.Huddleston H G, Quinn M M, Kao C N, Lenhart N, Rosen M P et al. (2017) Women with polycystic ovary syndrome demonstrate worsening markers of cardiovascular risk over the short-term despite declining hyperandrogenaemia: Results of a longitudinal study with community controls. Clin Endocrinol (Oxf). 87(6), 775-782.
- 6.Cussons A J, Stuckey B G, Walsh J P, Burke V, Norman R J. (2005) Polycystic ovarian syndrome: marked differences between endocrinologists and gynaecologists in diagnosis and management. Clin Endocrinol (Oxf). 62(3), 289-95.
- 7.J K Zawadzki, Dunaif A. (1992) Diagnostic criteria for polycystic ovary syndrome: toward a rational approach.in:A Dunaif. , JR Givens, F. Haseline. (Eds.).Polycystic ovary syndrome.Blackwell Scientific,Boston 377-384.
- 8. (2004) Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised (2003) consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. , Fertil Steril 81(1), 19-25.
- 9.Azziz R, Carmina E, Dewailly D, Diamanti-Kandarakis E, Escobar-Morreale H F et al. (2009) The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril. 91, 456-488.
- 10.Zhao Y, Qiao J. (2013) Ethnic differences in the phenotypic expression of polycystic ovary syndrome. Steroids. 78(8), 755-60.
- 11.Pazderska A, Kyaw Tun T, Phelan N, McGowan A, Sherlock M et al. (2018) In women with PCOS, waist circumference is a better surrogate of glucose and lipid metabolism than disease status per se. Clin Endocrinol (Oxf). 88(4), 565-574.
- 12.Huang X, Wang Q, Liu T, Pei T, Liu D et al. (2019) Body fat indices as effective predictors of insulin resistance in obese/non-obese polycystic ovary syndrome women in the Southwest of China. , Endocrine. Mar 65(1), 81-85.
- 13.Techatraisak K, Wongmeerit K, Dangrat C, Wongwananuruk T, Indhavivadhana S. (2016) Measures of body adiposity and visceral adiposity index as predictors of metabolic syndrome among Thai women with PCOS. Gynecol Endocrinol. 32(4), 276-80.
- 14.National Health and Nutrition Examination Survey (NHANES). Anthropometry Procedures Manual. Available at:- https://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/manual_an.pdf. Retrieved on:. 19-2019.
- 15.Goodman N, Bledsoe M, Cobin R, Futterweit W, Goldzieher J et al. (2001) E: "American Association of Clinical Endocrinologists Hyperandrogenism Guidelines". Endocrine Practice. 7(2), 120-134.
- 16.Guerrero-Romero F, Rodríguez-Morán M. (2003) Abdominal volume index. An anthropometry-based index for estimation of obesity is strongly related to impaired glucose tolerance and type 2 diabetes mellitus. Arch Med Res. 34(5), 428-32.
- 17.Thomas D M, Bredlau C, Bosy-Westphal A, Mueller M, Shen W et al. (2013) Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity (Silver Spring). 21(11), 2264-71.
- 18.Bergman R N, Stefanovski D, Buchanan T A, Sumner A E, Reynolds J C et al. (2011) A better index of body adiposity. Obesity (Silver Spring). 19(5), 1083-9.
- 19.Krakauer N Y, Krakauer J C. (2012) A new body shape index predicts mortality hazard independently of body mass index. PLoS One. 7(7), 1-10.
- 20.Valdez R. (1991) A simple model-based index of abdominal adiposity. , J Clin Epidemiol 44(9), 9556.
- 21.Morgante G, Cappelli V, A Di Sabatino, Massaro M G, V De Leo. (2015) Polycystic ovary syndrome (PCOS) and hyperandrogenism: the role of a new natural association. Minerva Ginecol. 67(5), 457-63.
- 22.Khomami M B, Tehrani F R, Hashemi S, Farahmand M, Azizi F. (2015) Of PCOS symptoms, hirsutism has the most significant impact on the quality of life of Iranian women. PLoS One. 10(4), 1-10.
- 23.Wong M, Zhao X, Hong Y, Yang D. (2014) Semiquantitative assessment of hirsutism. in 850 PCOS patients and 2,988 controls in China. Endokrynol Pol 65(5), 365-70.
- 24.Motta A B. (2012) The role of obesity in the development of polycystic ovary syndrome. Curr Pharm Des. 18(17), 2482-91.
- 25.González F, Considine R V, Abdelhadi O A, Acton A J. (2019) Oxidative stress in response to saturated fat ingestion is linked to insulin resistance and hyperandrogenism in PCOS. J Clin Endocrinol Metab. 12, 2019-00987.
- 26.Witchel S F, Burghard A C, Tao R H, Oberfield S E. (2019) The diagnosis and treatment of PCOS in adolescents: an update. Curr Opin Pediatr. 31(4), 562-569.
- 27.Spritzer P M, Motta A B. (2015) Adolescence and polycystic ovary syndrome: current concepts on diagnosis and treatment. Int J Clin Pract. 69(11), 1236-46.
- 28.Huang Z, Yong E L. (2016) Ethnic differences: Is there an Asian phenotype for polycystic ovarian syndrome? Best Pract Res Clin Obstet Gynaecol. 37, 46-55.
- 29.Wijeyaratne C N, Seneviratne Rde A, Dahanayake S, Kumarapeli V, Palipane E et al. (2011) Phenotype and metabolic profile of South Asian women with polycystic ovary syndrome (PCOS): results of a large database from a specialist Endocrine Clinic. Hum Reprod. 26(1), 202-13.
