Can Vitamin D Mitigate Osteoarthritic Hip Joint Arthroplasty Infections Among Older Adults? A Narrative Overview of the Literature Amidst COVID-19 Lockdowns and Beyond
Abstract
Background
Older adults with hip joint osteoarthritis, a major cause of chronic progressively disabling highly painful functional experiences, may require a surgical joint replacement procedure known as total joint arthroplasty surgery.
Objective
This review aimed to address the question of whether there an association between hip joint arthroplasty infection rates and prevailing pre or preoperative vitamin D levels that warrants consideration in efforts to prevent or minimize infection related hip arthroplasty complications among older adults particularly during the current ongoing COVID-19 pandemic.
Methods
PUBMED, SCOPUS, and WEB OF SCIENCE articles related to the topic and published between January 2016-2021 were searched, examined, and summarized.
Results
Older adults with hip joint osteoarthritis and low vitamin D serum levels who undergo total hip joint arthroplasty surgery may be at higher risk for post-operative infections than those with adequate vitamin D serum levels.
Conclusion
More research to verify whether efforts to screen for, and maximize vitamin D levels, before and after surgery, as indicated, may be helpful in the context of minimizing total hip joint arthroplasty surgery infection susceptibility and severity among older vitamin D deficient severely disabled hip osteoarthritis cases.
Author Contributions
Copyright © 2021 Ray Marks
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Hip joint osteoarthritis, a major cause of disabling pain among older adults, and predicted to occur in one of four older adults in the future 1, has long been considered a chronic health condition that deteriorates over time, and one that often requires surgical joint replacement, or a procedure known as total joint arthroplasty surgery. While commonly successful at reducing pain and increasing mobility 2, joint replacement surgery is not without complications such as joint infection, however 3. Indeed, while infection is not a given as a result of this form of surgery, it is cited to occur quite frequently in primary surgery contexts, as well as in cases requiring revision surgery, along with an array of possible undesirable outcomes and impacts 4. Moreover, even if only a small number of cases are likely to incur periprosthetic joint infections 5, given the immense additional social and personal costs and resultant suffering in the instance of a joint infection, substantive efforts to limit or reduce this occurrence and any further need for revision surgery has been advocated for some time. Indeed, while this situation, which is not easy to predict and resolve, remains a high priority issue for surgeons and hospitals, it is possible even more important to address in light of the ongoing COVID-19 pandemic where the patient may be in more severe pain and less healthy before surgery than in pre COVID-19 times 6.
In this regard, vitamin D, said to be a highly important hormone influencing many bodily functions that must be produced by the body in response to sunlight exposure or provided in supplement or food based formats, is cited as being required for fostering normal macrophage activity and inflammatory responses that may correlate with the presence of various modes of infection 7, 8, 9. Vitamin D may also impact on many physiological processes that have a link to osteoarthritis pathology 10, such as bone health 11. A role for vitamin D deficiency in the pathological processes underlying osteoarthritis can also not be ruled out. Thus, study of this possible association has not only been advocated, but appears to warrant attention, given the numbers of arthroplasty surgeries anticipated in the future, and the fact that prospective surgical candidates are commonly and predictably at high risk for vitamin D deficiencies 12 and likely to possibly be excessively impaired post COVID-19 lockdown situations. They may hence be more vulnerable to surgical infections than in pre pandemic times, as well as requiring prolonged rehabilitation periods due to COVID-19 related precautions and hospital administration changes that may excessively limit sunlight exposure.
To assure that those undergoing surgery in the face of the COVID-19 pandemic, do obtain significantly improved health, well-being and desired life quality status, it appears every effort to guard against unwanted postoperative joint infections should be made and is strongly warranted 3, 4, 5, 6.
In this respect, Morrison et al. 13 indicate that among an accepted array of precautionary practices, efforts to ensure vitamin D levels are not deficient (a term commonly referring to serum vitamin D levels of less than 20 ng/ml), may prove highly efficacious in minimizing the chances of unwanted post-operative joint infections, and their associated longer than desirable hospital stays. Accordingly, the current review reports on what is known about the role of vitamin D in the context of perioperative infections that continue to occur quite often following total joint replacement surgery 8.
The hip joint is examined as the sources of this dysfunction often require joint replacement surgery include hip fracture patients, who are often elderly with possible low vitamin D levels 9, as well as other prevailing health conditions that may correlate with vitamin D deficits such as obesity or frailty even if these are not directly associated with the disease incidence 2. The hip is also clearly a less well studied joint when compared to comparable data on knee joint arthroplasty infections and vitamin D.
Vitamin D is examined because it may yet have the potential to impact other important osteoarthritis correlates that may be associated in their own right with the disease and the patient’s ability to recover from hip joint surgery in a timely way, for example osteoporosis 14, possible fractures, and falls 10 see Box 1. The presence of insufficient vitamin D may also impact cartilage destruction, muscle atrophy, sarcopenic obesity, muscle strength, muscle recovery, and balance15, as well as arthroplasty surgery outcomes 12.
Box 1.Skeletal and Extra-Skeletal Correlates of Hip Osteoarthritis That Appear Impacted By Vitamin D Adequacy And Can Potentially Protect Against Poor Hip Osteoarthritis Surgery Outcomes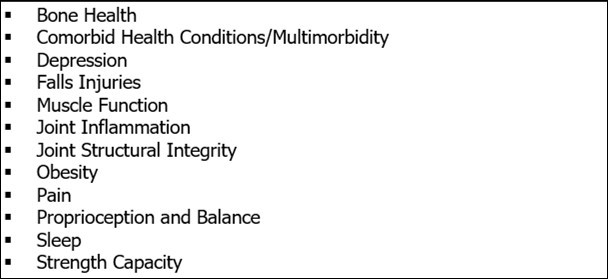
Significance
Hip joint osteoarthritis remains the most prevalent chronic disease disabler of older adults, and is a disease that frequently produces irreversible joint damage, along with varying degrees of oftentimes intractable pain, pain centralization or excess sensitivity that impacts cognitive wellbeing as well as functional ability. Despite years of research, very few remedies for successfully ameliorating this common progressive disabling disease prevail 16. Hence, many older adults and an increasing number of younger adults are forced to seek out the benefits of total joint replacement therapy, often very successfully, even if both hips require surgery at some point. Yet, some concern remains in the event the patient acquires an infection of their prosthetic device post surgery, which can prove debilitating, and often requires further surgery and costly care and additional hospitalization, from which a fair percentage of cases may not recover optimally.
It is also well established that many older adults with hip osteoarthritis also have osteoarthritis of other joints, such as the knee, as well as multiple comorbid health conditions, such as diabetes, that would possibly worsen their chances for an optimally envisioned post surgical outcome. Others may present solely with evidence of suboptimal vitamin D levels that could increase the risk for poor outcomes, including inflammation and infection levels, in general, in their own right, especially surgical outcomes 17.
Consequently, although occurring in only approximately 0.4-1.5% of hip arthroplasty cases 18, prosthetic joint infection that predictably produce costly, devastating outcomes after joint replacement surgery 19, 20, 21, 22 including re hospitalization, implant removal or exchange, and/or the prolonged use of potentially toxic and antimicrobial resistance-encouraging antibiotic 6 warrants attention. Indeed, despite many advances that have been made to reduce post-operative infection rates, Asaid et al. recently 20 noted that perioperative arthroplasty surgical infections continue to occur, and are rising in extent, rather than decreasing, in numbers 23.
Moreover, even if only small numbers of arthroplasty related joint infections are anticipated to occur in any given setting, the numbers must be considered substantive given that the total numbers of primary total hip arthroplasties to be carried out globally within the next two decades, is projected to exceed two million 24. This number may now be higher due to pandemic closures of elective surgery wards, as well as the pandemic itself that can be predicted to adversely impact overall well being. Even if not, dealing with technical complications such as infections post-operatively is now much more imperative than in pre COVID times, as well as being extremely costly to the patient, hospital and society, due to the greater virulence of hip infection microorganisms 25, 26. Since past research has failed to pinpoint exactly why some patients are at risk for infections after replacement surgery, and some are not, it seems worthwhile to continue to evaluate all possible preventable determinants that can be obviated, minimized, or tested and treated before and if needed after surgery. Since a considerable volume of literature implies a prevailing vitamin D deficiency may heighten post-operative complication risk following total hip replacement surgery, but these reviews generally included knee joint replacement data, a review focusing on perioperative infections specifically in hip osteoarthritis cases and its possible implications for those who perform surgical procedures, as well those undergoing these procedures seems timely 27.
Specific Aim
This review aimed to examine those recently published works that addressed the nature of vitamin D and its possible utility for helping to avert infections post hip joint arthroplasty. Suggestions as to how this data on vitamin D might be duly applied and advanced in the context of much needed efforts to maximize post operative hip joint replacement surgery recovery rates and magnitude, as well as avert excess surgical infection rates was specifically sought.
Methods
To achieve the overall aims of the current review, and to possibly answer the question of whether vitamin D is clinically relevant in the context of averting or minimizing post-operative hip arthroplasty infection rates, all pertinent articles listed on the PUBMED, Scopus, and Web of Science Consolidated Data Bases that appeared to inform about vitamin D, hip joint osteoarthritis, and post-surgical joint infections at the hip were sought and those of high relevance were examined specifically.
In this regard, topical articles published predominantly, in the last five years albeit not exclusively if an insightful report was relevant to the topic at hand, were examined and downloaded if deemed relevant. The research material reviewed was not restricted to any particular mode of inquiry, and both preclinical, as well as clinical data were considered relevant if they were peer reviewed full length articles published in English, and discussing vitamin D and its possible role in hip osteoarthritis, hip joint arthroplasty surgery infection outcomes. Articles referring solely to knee or other forms of osteoarthritis were excluded, as were non English articles.
After salient articles were scrutinized to examine if they addressed the present topic and questions of interest, those deemed relevant were selected for review, and discussed solely in narrative form as outlined below. In this regard, the term vitamin D was adopted throughout to describe this compound, mindful that diverse modes of vitamin D exist, along with its various properties, classifications, functional attributes, and typologies. The various modes of determining the extent of any prevailing vitamin D serum concentrations and their cutoff points and definitions of deficiency are reported as they appeared in the related literature, mindful that these are not necessarily uniform nor well standardized or accepted. The term COVID-19 is used to describe the novel corona virus that emerged in 2019 in Wuhan, China.
Results
The key terms outlined below, yielded a limited number of publications that covered the time periods January 1, 2016-December 30, 2020 as per Table 1.
Table 1. Summary of Numbers Related Studies On Key Data Bases Reviewed.| Key Terms Applied | PUBMED | WEB OF SCIENCE-5 data bases | SCOPUS |
| Hip Joint Arthroplasty + Vitamin D | 21 | 52 | 37 |
| Hip Joint Arthroplasty + Infection | 1942 | 2915 | 2448 |
| Hip Joint Replacement + Vitamin D | 16 | 62 | 33 |
| Hip Joint Replacement + Infection | 1503 | 2105 | 2055 |
| Infection, Hip Joint Arthroplasty + Vitamin D | 6 | 17 | 10 |
| Vitamin D + Osteoarthritis | 192 | 360 | 379 |
| Vitamin D + Joint Infection Prevention | 18 | 60 | 11 |
General Observations
Among the small number of available articles retrieved, a higher proportion than not tended to imply that vitamin D, a powerful hormone required to foster numerous vital physiological processes, may have a bearing on osteoarthritis progression and outcomes, and that its supplementary use in this regard may be helpful 16. Most however, did not focus on the possible role of adequate vitamin D in preventing osteoarthritis pain or ameliorating its severity, nor upon its possible impact on perioperative joint replacement infection rates.
In particular, while many studies have examined hip joint replacement surgery outcomes, as well as vitamin D and its role in possibly influencing hip arthroplasty surgical outcomes in their own right 28, 29, very few reports have tended to examine the possible influence of low vitamin D status or hypovitaminosis in mediating postsurgical infections of the osteoarthritic hip joint. Moreover, very few studies clearly prevail on this latter theme when compared to the analogous more widespread available data on vitamin D and knee joint arthroplasty infections, even though the topic may be especially relevant in the context of those surgeries conducted on older hip joint osteoarthritis patients who often present with multiple comorbid conditions 30.
Another point discussed by Dale et al. 31 is that that according to this group none of the risk factors they actively assessed could explain the increased risk for joint revision surgery due to infection, including male sex, hybrid fixation, cement without antibiotics, and surgery performed due to inflammatory disease, hip fracture, or femoral head necrosis, even when controlled for in their analysis. In contrast, they concluded that an increased incidence of prosthetic joint infection would therefore have to be caused by factors that were not examined in their study. They suggested these may include changes in patient-related factors, such as more comorbidity, changes in microbiology (i.e. increased bacterial virulence or more resistant strains), or changes in surgery-related factors (i.e. duration of surgery or changed surgical technique). They did not mention vitamin D or any other possible infection associated correlate, but stressed comorbidity, which can be traced in many cases to vitamin D deficiencies.
Eka et al. 32, too, who stressed the great importance of efforts to prevent joint arthroplasty related infections, failed to examine vitamin D as a possible risk factor, even though an absence of adequate vitamin D is found to mediate immune system responses negatively, and suboptimally 33. Another important overlooked vitamin D attribute may be its purported influence on pain, whereby its deficiency induces the excess use of pain medications believed to be possible predictors of worse COVID-19 disease manifestations 30 and thereby possibly of worse overall hip joint osteoarthritis outcomes.
According to Lavernia et al. 34 this set of possible related events, is noteworthy given that the prevalence of vitamin D insufficiency in cases undergoing hip arthroplasty surgery is purported to be approximately 30% (when using a 20 ng/mL cutoff value) and rises to 65% (when using a 30 ng/mL cutoff value), and that the subjects’ preoperative and postoperative functional scores were lower in those cases with insufficient vitamin D levels as determined using the 30 ng/mL cutoff value.
Specific Observations
As observed by Lavernia et al. 34, Piuzzi et al. 35 reported that high rates of vitamin D insufficiency and deficiency have indeed been evidenced in various patient populations, including those undergoing total joint arthroplasty surgery. In an effort to explore this issue, this group retrospectively identified 226 hip and knee patients who had undergone total joint replacement surgery and that had available data on vitamin D in their electronic medical records. After patients were stratified into vitamin D sufficient (≥30 ng/mL), insufficient (<30 ng/mL), and deficient groups (<20 ng/mL), results showed only 43.8% of cases were vitamin D sufficient. Unsurprisingly, Wall and De Steiger 12 concluded that attention to assessing vitamin D levels in advance of surgery appears highly warranted, especially during winter, and in light of the trend towards more negative surgical outcomes in those cases deemed vitamin D deficient prior to joint replacement surgery 36, 37, 38.
Hegde et al. 39 who clearly reiterated the fact that infection remains the most prevalent cause of joint arthroplasty failure despite recent advances, similarly proposed that vitamin D may be helpful in reducing this specific problem quite markedly. Accordingly, when this idea was examined in a mouse model, a vitamin D deficiency leading to an increased bacterial burden was observed. Moreover, the application of vitamin D supplementation reversed this situation. Subject to further study, a vitamin D deficiency may hence be a highly valuable and important potentially modifiable risk factor among older adults undergoing joint replacement as proposed by Alamanda and Springer 8 Arshi et al. 27, Maier et al 37 and Traven et al. 40.
Spinney et al. 41 too, who sought to determine whether vitamin D would be an effective modifiable nutritional marker for predicting postoperative infection risk and outcomes following prosthetic joint surgery concluded there is considerable evidence to support this view.
Likewise, Ginnetti et al. 42 observed that there was an association of note as regards a vitamin D deficiency and the development of postoperative joint surgery complications, such as an increased risk of infection. This is important to note especially in light of the current pandemic COVID-19, even though little attention has been given to this observation 43, when compared to other methods of addressing joint infections after surgery, such as the use of antibiotics 44, and evidence that hypovitaminosis-D is associated with higher complication rates, and a greater prevalence among septic versus aseptic revisions of the hip joint 45.
However, even though Papaioannou et al. 46 support the idea of vitamin D screening among the at risk elderly prior to orthopedic surgery, Signora et al. 47 who did indeed find a deficiency in vitamin D levels to prevail among their orthopedic patients, found that those with higher vitamin D levels, tended to be infected more readily than those with lower values. This situation has been identified to be of considerable concern, with some exceptions eg.51, as periprosthetic joint infections often require extensive revision surgery or prosthetic removal and replacement, that may lead to premature death 47, 48, 49, 50, and less favorable total joint arthroplasty outcomes than desired 40, 54, 55 See Figure 1.
Figure 1.Hypothesized Interactive Mechanisms In Face Of Vitamin D Deficits At Time Of Hip Joint Total Arthroplasty Surgery.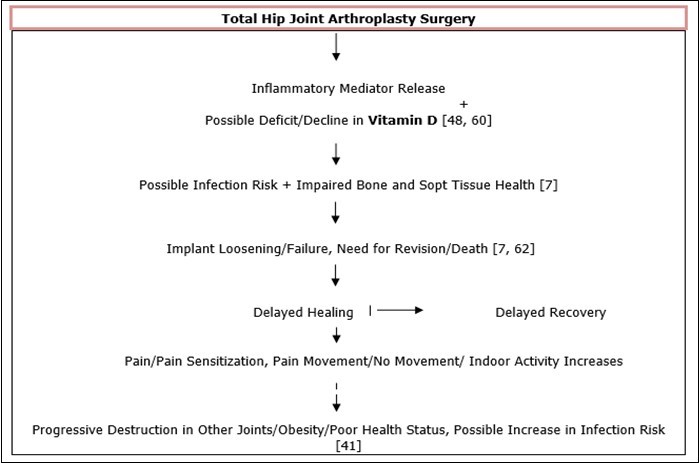
Discussion
Hip joint osteoarthritis is a widespread health condition, of high concern in the realm of efforts to optimize the wellbeing of older adults worldwide 1, 2, 30. Since treatments to alleviate the pain, inflammation, mechanical derangement, plus the weakening of joint muscles, bone, and cartilage 30 associated with hip osteoarthritis are often ineffective, surgical procedures are commonly advocated. However, as with all forms of surgery, complications such as infection remain among the most serious outcomes of these total hip joint arthroplasty surgeries 5, 7, 11, and that may lead to pain, debility, bone and sift tissue erosion, and implant loosening 7, as well as death 62 See Figure 1. This review sought to examine whether there is support for examining vitamin D serum levels among older adults undergoing this form of surgery, and offering vitamin D supplementation to mediate infection rates post hip joint arthroplasty in those adults found to be vitamin D deficient or at risk for a deficiency. A case for the utility of this idea was deemed highly necessary to undertake in light of the persistence of the COVID-19 pandemic where a substantive number of older patients may not only have deficient vitamin D levels 37, but worse hip joint disease manifestations prior to surgery than anticipated due to the impact of the COVID-19 lockdowns on pain, joint function, physical function, and physical activity in patients with end-stage hip osteoarthritis 6, 30. In addition, while in hospital they may be at greater risk than in pre pandemic times to infections 55, due to logistical factors, increased susceptibility, and possible care factors due to staff and resource shortages. Hypovitaminosis D, is also associated with increased susceptibility to frailty, falls, inactivity, and fractures 55. As such, this review, which examined almost all available current reports, revealed that a fair proportion of those older adults who require total hip arthroplasty surgery are likely to not only be vitamin D deficient, among exhibiting other debilitating health issues, but a small albeit important subgroup may sustain periprosthetic joint infections that delay healing and may require prolonged hospitalization and further surgery. On the other hand, efforts to attenuate postsurgical hip infection risk via the administration of vitamin D supplements as needed prior to joint arthroplasty surgery may be of high value in mitigating or averting both excess health deterioration and poorer than desired outcomes, as well as acute periprosthetic infections 48, along with the risk of hospitalization and severe COVID-19 49, 61.
Arguments against this idea however do prevail, and include, but are not limited to the idea that while baseline vitamin D levels do tend to decline post joint arthroplasty surgery, they also tend to return to baseline levels within six weeks as discussed by Binkley et al. 50. As well, Buirs et al. 51 discount vitamin D as having any bearing on the nature of total hip arthroplasty physical outcomes. This conclusion may arguably not apply to all cases, for example, those who sustain joint infections associated to some possible degree with low baseline vitamin D status or marginal status or other factors, such as the presence of one or more comorbid diseases 52, and/or a decline in vitamin D availability, other health issues or the presence of an overall compromised health status due this chronic situation 48. There is also an increasingly older population undergoing this form of surgery, that may at high risk for low vitamin D serum levels
In the meantime, even though neither Da Rocha et al. 30, nor Rhee et al. 53 mentioned vitamin D in their effort to advise osteoarthritis sufferers during this current ongoing COVID-19 pandemic, and this review may not have sourced all available publications, we agree with the conclusions of Wall and de Steiger 12 who argue that among the number of modifiable factors that increase the risk of postoperative complications following arthroplasty, one factor is the presence of a vitamin D deficiency. The degree to which outcomes are manifest post arthroplasty surgery may also depend on how close to desired levels the subject’s vitamin D status has been over time. Although not mentioned as a risk factor for perioperative infection specifically, Kong et al. 57 note that insufficient serum vitamin D concentrations are found to prevail in 40-65% of cases requiring total hip arthroplasty 58. As well, patients who go on to suffer from periprosthetic hip joint infections are found to have lower vitamin D levels than those who present with aseptic implant loosening complaints 59. Older adults who are candidates for hip joint arthroplasty surgery and who exhibit low vitamin D levels prior to surgery may also be expected to be at greater risk for worse postoperative outcomes, as well as infections, due to factors such as an associated functional decline and falls risk 60.
Consequently, while not conclusive, it is apparent that addressing this possible modifiable risk factor, as indicated, among others, not only over the course of helping the patient to manage their health condition more effectively, but especially prior to the implementation of hip joint arthroplasty surgery may yet help to reduce or hopefully eliminate the risk of adverse outcomes, in general, as well as the need for infection related revision surgery that often leads to premature death 40, 56. In addition, although more study is needed, parallel data show vitamin D is one important modifiable nutritional factor that is often deficient in the elderly, but one where repletion is a possible cost-effective and plausible approach to reducing postoperative infection risk among older adults scheduled to undergo joint arthroplasty surgery 11, 27, 45 as well as favorably impacting soft tissue healing and recovery, plus gait recovery, and length of hospital stay after surgery 63, 64, 65. To this end, and in light of projected increases in the incidence of costly periprosthetic infections among the elderly and their disastrous consequences 66, more extensive research to further a better understanding of the implications of vitamin D serum levels in the context of the health outcomes of adults 65 years of age and above who require hip joint replacement surgery 61 should be undertaken in the near future. This idea is clearly of high possible clinical significance in efforts to attain appropriate surgical outcomes 62, especially in the context of COVID-19, as well as the time period beyond that 66, 67, 68.
Conclusions
The need for hip joint arthroplasty surgery, which is likely to increase exponentially in the future may yet be impacted negatively in the case of a postsurgical infections, also projected to increase in numbers in the future.
Older adults with disabling hip osteoarthritis who are hip arthroplasty surgical candidates are more likely than not to benefit by efforts to uniformly examine and intervene as indicated to maximize their serum vitamin D levels prior to as well as following any arthroplasty surgery in this regard.
At the same time, adults 65 years of age or older who are diagnosed with hip osteoarthritis and who are asked to defer their scheduled joint replacement surgery appointments in response to COVID-19 lockdowns are likely to benefit from a standardized screening and supplementation effort, owing to the observed impact of isolation on vitamin D availability, and the risk posed by any deficiency towards on both COVID-19 risk, enforced hospitalization, plus possible worse than anticipated hip joint osteoarthritis outcomes.
On the other hand, early and timely administration of vitamin D as required by those older adults at risk for any vitamin D deficiency appears equally valuable for potentially averting surgical need, or in delaying this, while offering the best chances of a speedy safe surgical outcome, with less chance of revision, given the many attributes of vitamin D in the realm of joint health maintenance as well as overall health status.
References
- 1.Murphy L B, Helmick C G, Schwartz T A, Renner J B, Tudor G. (2010) One in four people may develop symptomatic hip osteoarthritis in his or her lifetime. , Osteoarthritis Cartilage 18, 1372-1379.
- 2.Murphy N J, Eyles J P, Hunter D J. (2016) Hip osteoarthritis: etiopathogenesis and implications for management. , Adv Ther 33(11), 1921-1946.
- 3.Schrama J C, Lutro O, Langvatn H, Hallan G, Espehaug B. (2012) Bacterial findings in infected hip joint replacements in patients with rheumatoid arthritis and osteoarthritis: a study of 318 revisions for infection reported to the Norwegian arthroplasty register. , ISRN Orthop 437675.
- 4.Schrama J C, Espehaug B, Hallan G, Engesaeter L B, Furnes O. (2010) Risk of revision for infection in primary total hip and knee arthroplasty in patients with rheumatoid arthritis compared with osteoarthritis: a prospective, population-based study on 108,786 hip and knee joint arthroplasties from the Norwegian Arthroplasty Register. Arthritis Care Res. 62, 473-479.
- 5.Ong K L, Kurtz S M, Lau E, Bozic K J, Berry D J. (2009) Prosthetic joint infection risk after total hip arthroplasty in the Medicare population. J Arthroplasty. Sep;24(6 Suppl): 105-9.
- 6.Endstrasser F, Braito M, Linser M, Spicher A, Wagner M. (2020) The negative impact of the COVID-19 lockdown on pain and physical function in patients with end-stage hip or knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 28(8), 2435-2443.
- 7.van Wijnen AJ, Abdel M P. (2017) Vitamin-D Supplementation: a low-risk, high-gain therapy to prevent PJI?: Commentary on an article by Vishal Hegde, MD, et al.: Single-dose, preoperative vitamin-D supplementation decreases infection in a mouse model of periprosthetic joint infection. , J Bone Joint Surg Am. Oct 99(20), 1-2.
- 8.Alamanda V K, Springer B D. (2019) The prevention of infection: 12 modifiable risk factors. , Bone Joint J. Jan;101-B(1_Supple_A): 3-9.
- 9.Hernigou P, Sitbon J, Dubory A, Auregan J C. (2019) Vitamin D history part III: the "modern times"-new questions for orthopaedic practice: deficiency, cell therapy, osteomalacia, fractures, supplementation, infections. , Int Orthop 43(7), 1755-1771.
- 10.Arima K, Mizukami S, Nishimura T, Tomita Y, Nakashima H. (2020) Epidemiology of the association between serum 25-hydroxyvitamin D levels and musculoskeletal conditions among elderly individuals: a literature review. , J Physiol Anthropol. Nov 39(1), 1-38.
- 11.Chan V W, Chan P K, Fu H, Cheung M H, Cheung A. (2020) Preoperative optimization to prevent periprosthetic joint infection in at-risk patients. , J Orthop Surg. Sep-Dec; 28(3), 1-8.
- 12.Wall C, R de Steiger. (2020) Pre-operative optimisation for hip and knee arthroplasty: Minimise risk and maximise recovery. , Aust J Gen Pract 49(11), 710-714.
- 13.RJM Morrison, Bunn D, Gray W K, Baker P N, White C. (2017) VASO (Vitamin D and Arthroplasty Surgery Outcomes) study - supplementation of vitamin D deficiency to improve outcomes after total hip or knee replacement: study protocol for a randomised controlled feasibility trial. , Trials. Nov 18(1), 514-10.
- 14.Glowacki J, Hurwitz S, Thornhill T S, Kelly M, LeBoff M S. (2003) Osteoporosis and vitamin-D deficiency among postmenopausal women with osteoarthritis undergoing total hip arthroplasty. , J Bone Joint Surg Am 85(12), 2371-7.
- 15.Krasowska K, Skrobot W, Liedtke E, Sawicki P, Flis D J. (2019) The preoperative supplementation with vitamin d attenuated pain intensity and reduced the level of pro-inflammatory markers in patients after posterior lumbar interbody fusion. Front Pharmacol. 22, 1-8.
- 17.Brambilla L, Peretti G M, Sirtori P, Maffulli N, Mangiavini L. (2020) Outcome of total hip and total knee arthroplasty and vitamin D homeostasis. , Br Med Bull. Oct 135(1), 50-61.
- 18.Memtsoudis S G, Ma Y, A Gonzalez Della Valle, Besculides M C, Gaber L K. (2010) Demographics, outcomes, and risk factors for adverse events associated with primary and revision total hip arthroplasties in the United States. , Am J Orthop 39, 72-77.
- 19.Dowsey M M, Choong P F. (2008) Obesity is a major risk factor for prosthetic infection after primary hip arthroplasty. , Clin Orthop Relat Res 466, 153-158.
- 20.Asaid R, Williams I, Hyde D, Tiang T. (2012) Infection rates following hip and knee joint arthroplasty: large referral centre versus a small elective-only hospital. , Eur J Orthop Surg Traumatol 23, 165-168.
- 21.Dale H, Skråmm I, Løwer H L, Eriksen H M, Espehaug B. (2011) Infection after primary hip arthroplasty: a comparison of 3 Norwegian health registers. , Acta Orthop 82, 646-654.
- 22.Peel T N, Cheng A C, Choong P F.Buising KL (2012). Early onset prosthetic hip and knee joint infection: treatment and outcomes in Victoria. , Australia. J Hosp Infect 82, 248-253.
- 23.Ahmed S S, Yaghmour K M, Haddad F S. (2020) The changing face of infection, diagnosis, and management in the United Kingdom. Orthop Clin North Am. 51(2), 141-146.
- 25.Kapadia B H, Berg R A, Daley J A, Fritz J, Bhave A. (2016) Periprosthetic joint infection. , Lancet. Jan 387(10016), 386-394.
- 26.Efremov K, Benedetti Valentini M, F De Maio, Potenza V, Caterini R. (2019) Periprosthetic hip and knee infections: comparison of etiology, perioperative management and costs. Eur Rev Med Pharmacol Sci. Apr;23(2 Suppl): 217-223.
- 27.Arshi A, Shieh A, Adams J S, Bernthal N M, Zeegen E N. (2020) Preoperative vitamin D repletion in total knee arthroplasty: a cost-effectiveness model. , J Arthroplasty 35(5), 1379-1383.
- 28.Jansen J, Tahmassebi J, Haddad F S. (2017) Vitamin D deficiency is associated with longer hospital stay and lower functional outcome after total knee arthroplasty. , Acta Orthop Belg 83(4), 664-670.
- 29.Zhang H, Zhu X H, Dong W, Wang Q M. (2018) Vitamin D status and patient outcomes after knee or hip surgery: a meta-analysis. , Ann Nutr Metab 73(2), 121-130.
- 30.FA Castro da Rocha, LDP Melo, Berenbaum F. (2020) Tackling osteoarthritis during COVID-19 pandemic Ann Rheum Dis.
- 31.Dale H, Fenstad A M, Hallan G, Havelin L I, Furnes O. (2012) Increasing risk of prosthetic joint infection after total hip arthroplasty. , Acta Orthopaedica 83, 449-458.
- 32.Eka A, Chen A F. (2015) Patient-related medical risk factors for periprosthetic joint infection of the hip and knee. , Ann Transl Med 3(16), 1-12.
- 33.Siddiqui M, Manansala J S, Abdulrahman H A, Nasrallah G K, Smatti M K. (2020) Immune modulatory effects of vitamin D on viral infections. , Nutrients. Sep 12(9), 2879-10.
- 34.Lavernia C J, Villa J M, Iacobelli D A, Rossi M D. (2014) Vitamin D insufficiency in patients with THA: prevalence and effects on outcome. Clin Orthop Relat Res. 472(2), 681-6.
- 35.Piuzzi N S, George J, Khlopas A, Klika A K, Mont M A. (2018) High prevalence and seasonal variation of hypovitaminosis D in patients scheduled for lower extremity total joint arthroplasty. , Ann Transl Med. Aug; 6(16), 1-7.
- 36.Nawabi D H, Chin K F, Keen R W, Haddad F S. (2010) Vitamin D deficiency in patients with osteoarthritis undergoing total hip replacement: a cause for concern?. , J Bone Joint Surg Br 92(4), 496-9.
- 37.Maier G S, Horas K, Seeger J B, Roth K E, Kurth A A. (2014) Is there an association between periprosthetic joint infection and low vitamin D levels?. , Int Orthop 38(7), 1499-504.
- 38.P J Iglar, K J Hogan. (2015) Vitamin D status and surgical outcomes: a systematic review. Patient Saf Surg. 9(14), 1-10.
- 39.Hegde V, Dworsky E M, Stavrakis A I, Loftin A H, Zoller S D. (2017) Single-dose, preoperative vitamin-D supplementation decreases infection in a mouse model of periprosthetic joint infection. , J Bone Joint Surg Am. Oct 99(20), 1737-1744.
- 40.Traven S A, Chiaramonti A M, Barfield W R, Kirkland P A, Demos H A. (2017) Fewer complications following revision hip and knee arthroplasty in patients with normal vitamin D levels. , J Arthroplasty. Sep; 32(9), 193-196.
- 41.Spinney E. (2020) Vitamin D as a preoperative clinical predictor for prosthetic joint infection. , JBJS J Orthopaedics for Physician Assistants: 8(2).
- 42.Ginnetti M, El-Othmani M M, Wright E, Tzeng T H, Saleh J. (2016) Effect of vitamin D on joint replacement outcomes. , Instr Course Lect 65, 521-530.
- 43.Galmés S, Serra F, Palou A. (2020) Current state of evidence: influence of nutritional and nutrigenetic factors on immunity in the COVID-19 pandemic Framework. , Nutrients. Sep 12(9), 1-34.
- 44.Çimen O, Azboy N, Çatal B, Azboy İ. (2020) Assessment of periprosthetic joint infection prevention methods amongst Turkish orthopedic surgeons in total joint replacement: a survey. Jt Dis Relat Surg. 31(2), 230-237.
- 45.Emara A K, Nageeb E, George J, Buttaro M A, Higuera C. (2020) Hypovitaminosis D in lower extremity joint arthroplasty: a systematic review and meta-analysis. , J Orthop. Mar 25, 109-116.
- 46.Papaioannou I, Pantazidou G, Kostoglou-Athanasiou I, Korovessis P. (2020) Hypovitaminosis D in the Greek elderly population doesn't concern only patients with hip fracture. , Cureus. Aug 12(8), 1-11.
- 47.Signori V, Romanò C L, E De Vecchi, Mattina R, Drago L. (2015) osteoarticular infections be influenced by vitamin D status? An observational study on selected patients. , BMC Musculoskelet Disord. Aug 5, 1-5.
- 48.Zajonz D, Prager F, Edel M, Möbius R, Daikos A. (2018) The significance of the vitamin D metabolism in the development of periprosthetic infections after THA and TKA: a prospective matched-pair analysis of 240 patients. , Clin Interv Aging. Aug 17, 1429-1435.
- 49.Mendy A, Apewokin S, Wells A A, Morrow A L. (2020) Factors associated with hospitalization and disease severity in a racially and ethnically diverse population of COVID-19 patients. medRxiv [Preprint]. 27, 1-25.
- 50.Binkley N, Coursin D, Krueger D, Iglar P, Heiner J. (2017) Surgery alters parameters of vitamin D status and other laboratory results. , Osteoporos Int 28(3), 1013-1020.
- 51.Buirs L D, Van Beers LW, Scholtes V A, Pastoors T, Sprague S. (2016) Predictors of physical functioning after total hip arthroplasty: a systematic review. , BMJ Open. Sep 6(9), 1-7.
- 52.Bozic K J, Lau E, Steven Kurtz, Ong K, Rubash H. (2012) Patient-related risk factors for periprosthetic joint infection and postoperative mortality following total hip arthroplasty in medicare patients. , J Bone & Joint Surg 94(9), 794-800.
- 53.Rhee C, Lethbridge L, Richardson G, Dunbar M. (2018) Risk factors for infection, revision, death, blood transfusion and longer hospital stay 3 months and 1 year after primary total hip or knee arthroplasty. , Can J Surg 61(3), 165-176.
- 54.Lang P O, Samaras N, Samaras D, Aspinall R. (2013) How important is vitamin D in preventing infections?. , Osteoporos Int 24, 1537-1553.
- 55.Tramontana F, Napoli N, El-Hajj Fuleihan G, Strollo R. (2020) The D-side of COVID-19: musculoskeletal benefits of vitamin D and beyond. , Endocrine 69(2), 237-240.
- 56.Gundtoft P H. (2017) Prosthetic Joint Infection following total hip arthroplasty - incidence, mortality and validation of the diagnosis in the Danish Hip Arthroplasty Register. , Dan Med J. Sep; 64(9), 5397.
- 57.Kong L, Cao J, Zhang Y, Ding W, Shen Y. (2017) Risk factors for periprosthetic joint infection following primary total hip or knee arthroplasty: a meta-analysis. , Int Wound J 14(3), 529-536.
- 58.Visser E, de Roos NM, Oosting E, Endenburg S C, Dronkers J J. (2018) Association between preoperative vitamin D status and short-term physical performance after total hip arthroplasty: a prospective study. , Ann Nutr Metab 73(3), 252-260.
- 59.Kenanidis E, Kakoulidis P, Karponis D, Tsiridis E. (2020) The effect of perioperative vitamin D levels on the functional, patient-related outcome measures and the risk of infection following hip and knee arthroplasty: a systematic review. Patient Relat Outcome Meas. 11, 161-171.
- 60.Foccillo A, Aicale R, Maffulli N. (2018) Elective orthopaedic and trauma patients in Southern Italy are vitamin D deficient. a pilot study. , Transl Med UniSa 17, 6-11.
- 61.Ragni E, Mangiavini L, Viganò M, Brini A T, Peretti G M. (2020) . Management of osteoarthritis during the COVID-19 pandemic. Clin Pharmacol Ther 108(4), 719-729.
- 62.Berend K R, Lombardi AV Jr, Morris M J, Bergeson A G, Adams J B. (2013) Two-stage treatment of hip periprosthetic joint infection is associated with a high rate of infection control but high mortality. Clin Orthop Relat Res. 471(2), 510-8.
- 63.Moon A S, Boudreau S, Mussell E, He J K, Brabston E W. (2019) Current concepts in vitamin D and orthopaedic surgery. Orthop Traumatol Surg Res. , Apr; 105(2), 375-382.
- 64.da Cunha BM, Gava A D, de Oliveira SB, de David AC, Dos Santos-Neto LL. (2016) Vitamin D is related to gait recovery after total hip arthroplasty: a prospective analysis. Gait Posture. Oct;50: 96-101.
- 65.Maier G S, Maus U, Lazovic D, Horas K, Roth K E. (2016) Is there an association between low serum 25-OH-D levels and the length of hospital stay in orthopaedic patients after arthroplasty?. , J Orthop Traumatol 17(4), 297-302.
- 66.Chang C H, Lee S H, Lin Y C, Wang Y C, Chang C J. (2020) Increased periprosthetic hip and knee infection projected from 2014 to 2035 in Taiwan. , J Infect Public Health 13(11), 1768-1773.
