Significance of Radiological Findings in Patients with Respiratory and Abdominal Manifestations of Covid-19
Abstract
The autopsy findings of patients died from Covid -19 showed that pulmonary and multiorgan small vessels thromboembolism is an essential features of the disease.
Small vessels thromboembolism is frequently not detected by means of laboratory and radiological investigations.
The current perspective reviewed the different radiological findings in patients with covid -19 suffering from respiratory and/or abdominal symptoms and also reviewed the recent studies which used the contrast enhanced ultrasound in the diagnosis of patients with pulmonary and multiorgan small vessels thrombosis.
Author Contributions
Academic Editor: Mohammed Ali Chowdhury, Hubei University for Nationalities, China.
Checked for plagiarism: Yes
Review by: Single-blind
Copyright © 2021 Ashraf Talaat Youssef
 This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Competing interests
The authors have declared that no competing interests exist.
Citation:
Introduction
Covid -19 pandemic, is an ongoing global pandemic which is caused by SARS-CoV-2. Currently more than 190 million cases have been confirmed with more than 4 million deaths, making it one of the deadliest pandemics in the history. Up to now, no effective treatment was detected and nearly 14 % of the world population were vaccinated 1.
A literature review of 28 scientific papers which published the autopsy findings of patients died from Covid-19 with total number of cases is 341, concluded that the major histological findings in the lung is diffuse alveolar damage with hyaline membrane formation, and microthrombi in small pulmonary vessels 2.
It appears that there is a high incidence of deep vein thrombosis of an estimated %14.8% among the hospitalized patients which are risky for pulmonary embolism.
Pulmonary thromboembolism signifies the presence of severe covid-19, may lead to respiratory failure and necessitates patient hospitalization and if multiple will suggest bad prognosis 3.
Small vessels thrombosis may be followed by large vessel thrombosis or recurrent pulmonary thromboembolism. The estimated mortality rate in cases with recurrent pulmonary thromboembolism was about 45%.
Multiorgan damage frequently detected and was associated with hyperinflammatory response and fibrinous thrombi of the small vessels of liver, kidneys, heart and bowel 2.
An immune related thromboembolism in patients with Covid-19 was associated with hypercoagulability state, platelet dysfunction, platelet aggregation and vascular endotheliitis 4.
D-dimer and ventilation /perfusion scan are of high sensitivity and low specificity in the detection of pulmonary thromboembolism.
Computed tomography pulmonary angiography (CTPA) can’t evaluate the microcirculation. Nephrotoxicity, radiation exposure and the patient critical condition are considered limitations to the use of CTPA. CTPA can detect only large and medium pulmonary vessels thrombosis and subsequent pulmonary infarction 3, 5.
Echocardiography can show sequalae of massive pulmonary embolism by detecting right ventricular dilation, tricuspid valve regurge, pulmonary hypertension and Rt ventricular apical dyskinesia 6.
So, radiologists are in urgent need to an effective imaging modality capable of detecting micro vessels thrombosis with subsequent ischemia and infarctions.
Contrast enhanced ultrasound is an imaging modality which was used recently to detect small vessels thrombosis with subsequent organ ischemia and infarction in patients of Covid-19 showing promising results 5, 7, 8, 9, 10, 11.
Radiological Findings in Cases with Covid -19 Respiratory Symptoms
Covid -19 initially leads to tracheobronchitis of upper respiratory tract.
When the infections extend to the lower respiratory tract, the virus will attack pneumocytes type 2, mainly located at the periphery of lung fields in subpleural regions which explains the classic distribution of the ground glass opacity and consolidation found in chest CT.
Chest CT findings in patients with Covid-19 include mainly bilateral and peripheral patchy areas of ground glass opacities, patchy areas of consolidation, linear opacities, Crazy paving pattern, halo sign and reverse halo sign. Bilaterality observed in late disease. Pleural, pericardial effusion and lymphadenopathy are rare findings 12.
Cases with severe Covid-19 were found with diffuse alveolar damage subsequent of immune hyperinflammatory reaction, the effect of viral infection as well as pulmonary thromboembolism.
Patients with severe Covid-19 and lower respiratory tract symptoms can be initially evaluated with bed side chest ultrasound under complete protective measures.
Bed side chest ultrasound may reveal positive findings as multiple Kerley’s B lines (>3 per intercostal space), pleural wall thickening (Figure 1), patchy areas of pulmonary consolidations especially in subpleural location (Figure 2, Figure 3) and obstructive lung collapse.
Figure 1.Real time chest ultrasound showing Kerley’s B lines in patient with covid -19.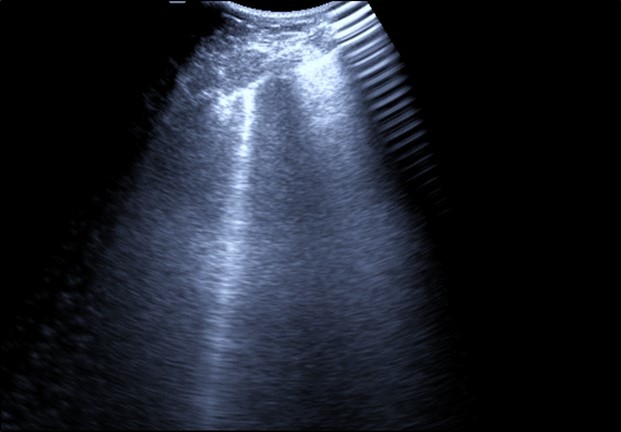
Figure 2.Chest ultrasound showing subpleural consolidation in patient with Covid-19.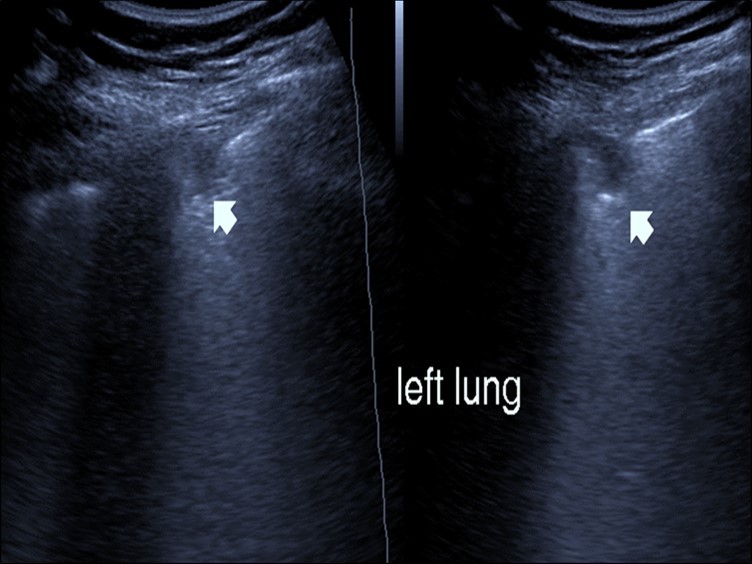
Figure 3.Chest ultrasound showing right lung segmental consolidation with positive air bronchogram.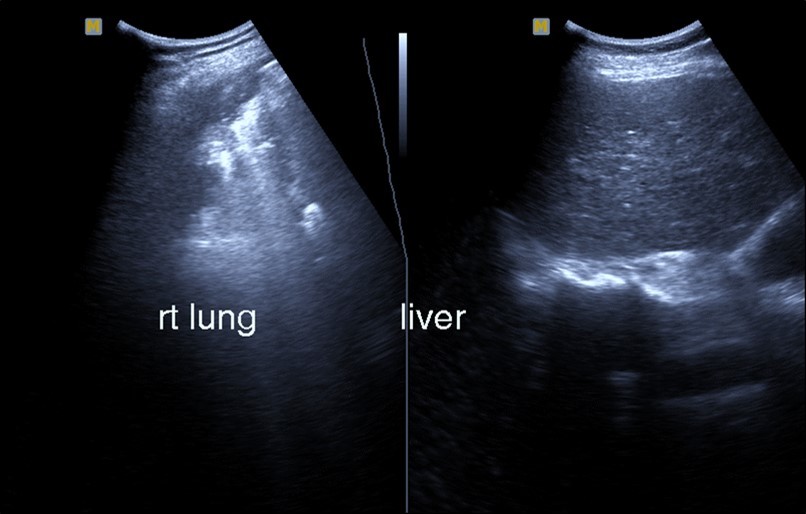
Recently contrast enhanced ultrasound with few trials used to image the target areas after being located with B.mode US followed by Contrast US enhancement exam after injection of 1.8-2.5mm of the contrast agent followed by 5-10 CC saline flush to allow the distribution of contact agent through the circulation. The target areas were evaluated for the pattern of contrast enhancement 7, 8, 9, 10, 11.
Hyperenhancement suggests inflammatory consolidation while absent or hypo enhancement will suggest infarction. Early recognition of hypoechoic areas as lung infarction rather than inflammatory consolidation with CEUS can provide prognostic and diagnostic information to guide early management. CEUS also allowed to demonstrate revascularization during recovery 5.
Patients with Abdominal Manifestations of Covid-19 May Suffer from
Hepatic impairment.
Biliary stasis and acute cholecystitis.
Renal impairment.
Suprarenal gland infarctions.
Splenic infarctions.
Acute pancreatitis
Bowel wall inflammation, mesenteric vascular occlusion with subsequent intestinal ischemia and infarctions 2, 13, 14.
Initially, real time abdominal ultrasound exam was performed, followed by power or color duplex ultrasound for the evaluation of abdominal vessels. The areas of interest can be further examined with contrast enhanced ultrasound exam to evaluate the microcirculation
Abdominal ultrasound may revealed any of the followings:-Mild hepatomegaly with echogenic parenchyma and ascites in cases with hepatic impairment (Figure 4, Figure 5) ,thick walls of gall bladder with mildly dilated Common bile duct suggesting of biliary stasis and cholecystitis (Figure 6) .Abnormal renal echogenicity (Figure 7), suprarenal gland enlargements with heterogeneous texture ,splenic wedge shape area of hypoechogenicity ,thickened walls of bowel mainly the rectosigmoid region ,dilated bowel loops with free peritoneal fluid, and gases in the bowel wall with mesenteric and portal vein gases suggesting of bowel wall infarction13.
Figure 4.Real time ultrasound showing thickened wall of gall bladder (gb) with dilated Common bile duct (cbd) in patient with severe Covid-19.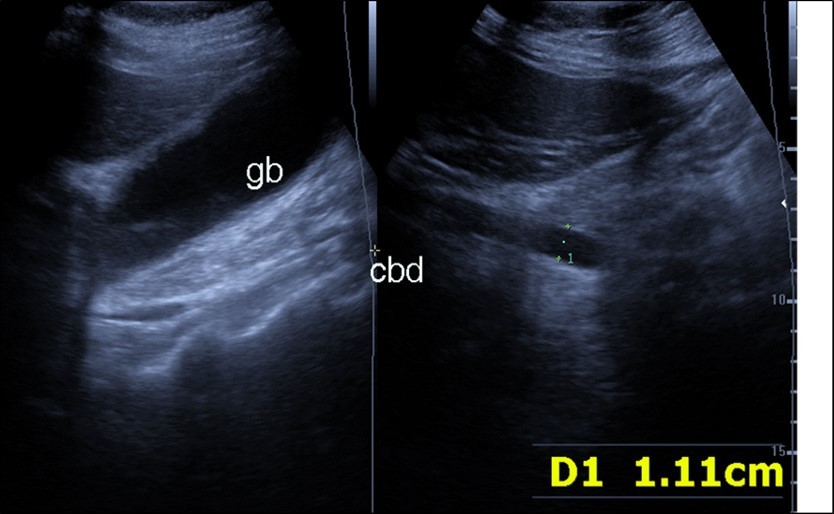
Figure 5.Real time ultrasound showing mild hepatomegaly (li), ascites and thickened gall bladder wall(gb).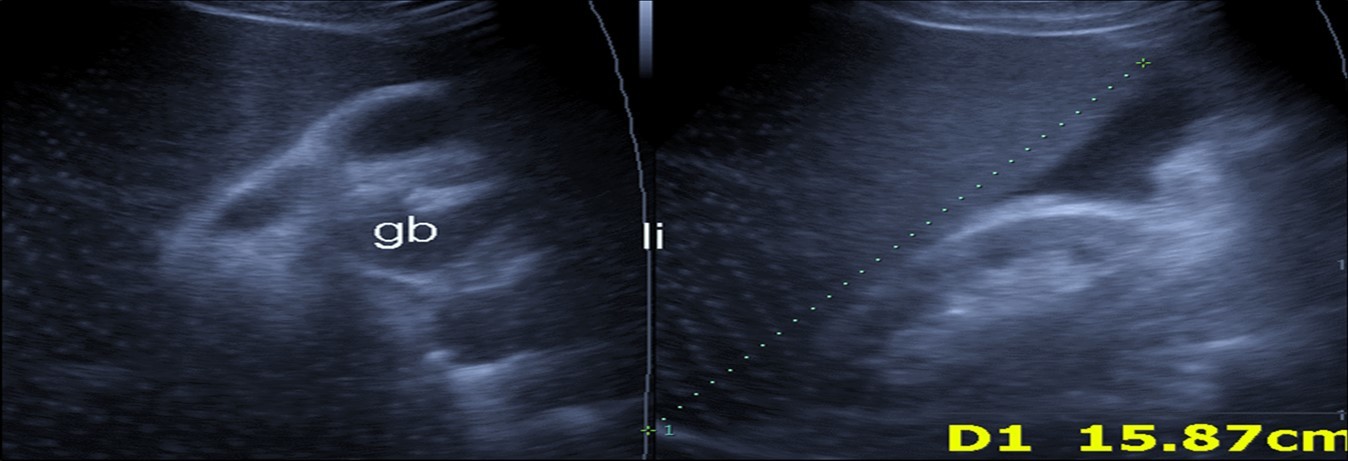
Figure 6.Real time ultrasound showing free ascites (asc) in patient with Covid-19.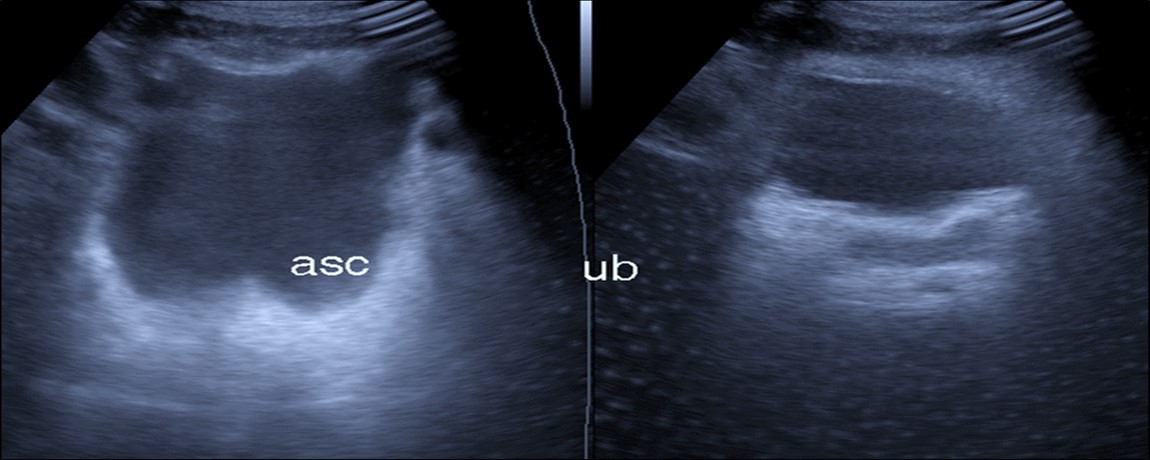
Figure 7.Patient with Covid-19 showing an echogenic kidney (rk) by ultrasound.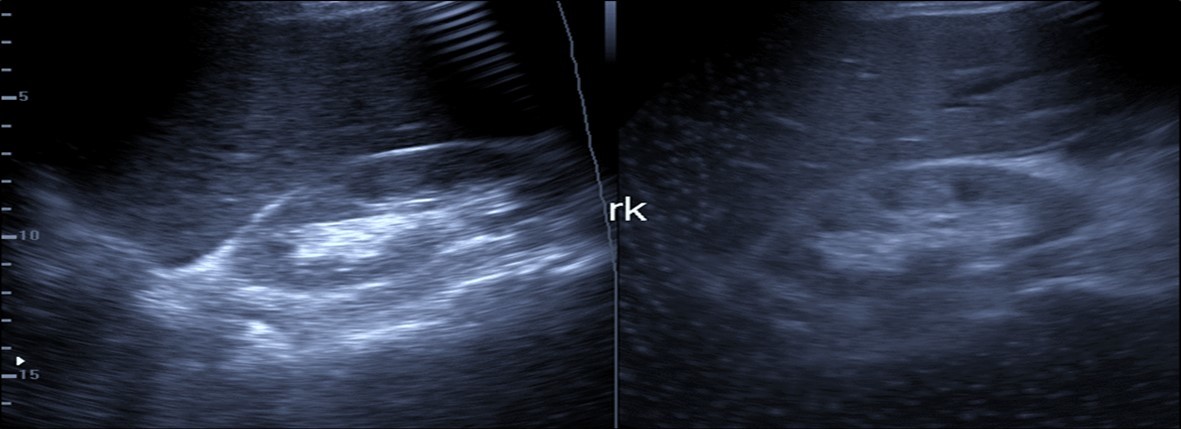
Contrast Enhanced Ultrasound May Reveal
1. Patchy areas of hyperenhancement in the liver corresponding to hyperinflammatory response. Attenuated course of hepatic artery branches with subcapsular lack of contrast enhancement suggesting of hepatic ischemia.
2. Thick walls of gall bladder with increased enhancement suggesting of cholecystitis
3. Increased renal parenchymal enhancement with acute tubular injury versus collapsing glomerulonephropathy and focal areas of reduced cortical enhancement associated with small renal vessels microthrombosis.
4. Enlarged suprarenal glands with reduced or absent enhancement denoting suprarenal gland infarctions.
5. Areas of no enhancement in the spleen suggesting of infarctions 14.
6. Hyperenhancment of bowel walls associated with bowel wall inflammation or focal areas of no enhancement in the bowel walls suggesting of intestinal wall infarctions.
Discussion
Small vessels thromboembolism is frequently undetected by means of radiological and laboratory investigations, in spite being a main feature of Covid-19 proved by the few radiology trials of using the ultrasound contrast enhancement and the autopsy findings of patients died from Covid-19 2, 7, 8, 9, 10, 11.
Small vessels thromboembolism is multifactorial, caused by coagulopathy, thrombocytopathy and endotheliopathy associated with severe Covid -19.
Endotheliitis can be resulted from direct viral infection of the endothelial cells or immune hyperinflammatory reaction. The hypothesis of direct viral infectivity was opposed by the recent findings of scanty ACE- 2 receptors on the endothelium cells and the recent study which showed inability of the virus to infect cultured endothelium cells, raising the possibility of being subsequent of the hyperinflammatoy reaction 15.
Abnormal coagulation profile and platelet dysfunction in patients with severe Covid -19 in conjunction with endotheliopathy will lead to the frequent finding of small vessels thromboembolism among the patients 4, 15.
The United Kingdom SARS corona virus-2 variant was found to be associated with high incidence of vasculopathy compared with the old variants with high incidence of vasculitis and perivascular fat planes inflammation. The mortality rate in hospitalized patients with vasculopathy was three-fold higher than patients without vasculopathy. The mortality rate in patients who received dexamethasone therapy was three times less than in patients who didn’t receive dexamethasone. The estimated hazard ratio in patients with vasculopathy and didn’t receive dexamethasone was 8.24 compared with those without vasculopathy 16.
The forementioned findings demonstrate the success of dexamethasone in management of vasculitis.
Management of small vessels thromboembolism was assumed to depend on the use Gluco-corticosteroid (Dexamethasone) therapy, antiviral drugs and anticoagulants.
In ophthalmology Cytomegalo-virus corneal endotheliitis was successfully managed with antiviral drugs, and topical corticosteroids 17.
Endotheliitis in covid -19 patients can be treated with corticosteroid therapy, anticoagulant and antiviral therapy. Prostacycline fatty acid derivative of Arachidonic acid can be useful as it promotes the healing of endothelium, vasodilator and prevent platelets aggregation (4).
Omega -3 fatty acid can be helpful as it promotes the healing of endothelium, inhibit the platelet aggregation and can switch off the cytokines storm 18.
Conclusion
Small vessels thromboembolism is an essential feature of Covid-19 which is frequently undetected by means of radiological and laboratory investigations, mainly caused by endotheliitis, coagulopathy and thromocytopathy. Prevention and early management will help greatly to reduce the severity of the disease and mortality rate.
Funding: None
Acknowledgements
None
References
- 1. (2019) World Health Organization. Coronavirus disease2019(COVID-19) Situation Report,23july2021In: World Health Organization [Internet]. Available from: https://reliefweb.int/report/world/coronavirus-disease-2019-covid-19-situation-report.
- 2.Maiese A, Manetti A C, La Russa R. (2021) Autopsy findings in COVID-19-related deaths: a literature review. Forensic Sci Med Pathol. 17(2), 279-296.
- 3.Young Joo Suh.Hyunsook Hong, Mickaël Ohana, Florian Bompard, Marie-Pierre Revel, Clarissa Valle, et al. (2021).Pulmonary Embolism and Deep Vein Thrombosis in COVID-19: A Systematic Review and Meta-Analysis.Radiology 298, 70-80.
- 4.S X Gu, Tyagi T, Jain K. (2021) Thrombocytopathy and endotheliopathy: crucial contributors to COVID-19 thromboinflammation. , Nat Rev Cardiol 18, 194-209.
- 5.Yusuf G T, Wong A, Rao D, Tee A, Fang C et al. (2020) . The use of contrast-enhanced ultrasound in COVID-19 lung imaging.Ultrasound 1-5.
- 6.Kurnicka K, Lichodziejewska B, Goliszek S, Dzikowska-Diduch O, Zdończyk O et al. (2016) Echocardiographic Pattern of Acute Pulmonary Embolism: Analysis of 511 Consecutive Patients. J Am Soc Echocardiogr. Sep;29(9): 907-13. doi: 10.1016/j.echo.2016.05.016. Epub2016Jul15.PMID: 27427291.
- 7.Peng Q, Wang X, Zhang L. (2020) Findings of lung ultrasonography of novel corona virus pneumonia during the 2019–2020 epidemic. Intensive Care Med.
- 8.Zotzmann V, Lang C N, Bamberg F. (2020) Are subpleural consolidations indicators for segmental pulmonary embolism in COVID-19? Intensive Care Med.
- 9.Henry B M, Vikse J, Benoit S, Favaloro E J, Lippi G. (2020) Hyperinflammation and derangement of renin-angiotensin-aldosterone system in COVID-19: A novel hypothesis for clinically suspected hypercoagulopathy and microvascular immunothrombosis. , Clin Chim Acta 507, 167-173.
- 10.Pastor S. (2017) Detection of peripheral embolic consolidations using contrast-enhanced ultrasonography in patients with no evidence of pulmonary embolism on computed tomography: A pilot study. , J Clin Ultrasoun JCU 45(9), 575-579.
- 11.Trenker C, Dohse M, Ramaswamy A, Michel C, Görg C. (2019) Histological validation of pulmonary infarction detected with contrast-enhanced ultrasound in patients with negative computed tomography pulmonary angiogram: a case series. J Clin Ultrasound JCU 47(8): 461–H-209003 PMCID: PMC7369109PMID: 32333581.
- 12.Li J, Yan R, Zhai Y, Qi X, Lei J.Chest CT findings in patients with coronavirus disease 2019 (COVID-19): a comprehensive review. Diagn Interv Radiol.2020Nov2.doi: 10.5152/dir.2020.20212.Epub ahead of print.PMID:. 33135665.
- 13.Vaidya Tanvi, Nanivadekar Avinash, Patel Rajan. (2021) Imaging spectrum of abdominal manifestations of COVID-19. , World J Radiol 13(6), 157-170.
- 14.Jung E M, Stroszczynski C, Jung F. (2020) Contrast enhanced ultrasonography (CEUS) to detect abdominal microcirculatory disorders in severe cases of COVID-19 infection: First experience. , Clin Hemorheol Microcirc 74(4), 353-361.
- 15.Nicosia R F, Ligresti G, Caporarello N, Akilesh S, Ribatti D. (2021) COVID-19 Vasculopathy: Mounting Evidence for an Indirect Mechanism of Endothelial Injury. Epub2021May23. PMID: 34033751; PMCID: PMC8141344 , Am J Pathol 191(8), 1374-1384.
- 16.Davenport Liam. (2021) COVID-19-induced Vascular Inflammation Behind Mortality. Risk:June14,2021 British Cardiovascular Society2021Annual Conference: The UK COVID-19 Cardiovascular CT Risk Assessment Consortium .